Abstract
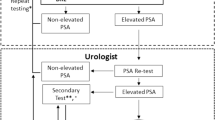
Early identification and management of prostate cancer completely changed with the discovery of prostate-specific antigen. However, improved detection has also led to overdiagnosis and consequently overtreatment of patients with low-risk disease. Strategies for the management of patients using active surveillance — the monitoring of clinically insignificant disease until intervention is warranted — were developed in response to this issue. The success of this approach is critically dependent on the accurate selection of patients who are predicted to be at the lowest risk of prostate cancer mortality. The Epstein criteria for clinically insignificant prostate cancer were first published in 1994 and have been repeatedly validated for risk-stratification and selection for active surveillance over the past few decades. Current active surveillance programmes use modified criteria with 30–50% of patients receiving treatment at 10 years. Nonetheless, tools for prostate cancer diagnosis have continued to evolve with improvements in biopsy format and targeting, advances in imaging technologies such as multiparametric MRI, and the identification of serum-, tissue- and urine-based biomarkers. These advances have the potential to further improve the identification of men with low-risk disease who can be appropriately managed using active surveillance.
Key points
-
The current prostate cancer treatment paradigm relies on accurate identification and risk stratification for patients who need immediate intervention versus active surveillance.
-
Epstein criteria for low-risk disease were developed in 1994 and, despite advances in biopsy templates and pathological definitions, the criteria have demonstrated durability over time.
-
Developments in MRI and consequently targeted prostate biopsy have improved cancer detection, especially in anterior tumours. As further research in diagnostic imaging is carried out, this technology may have an increased role in active surveillance protocols.
-
A growing body of research into novel biomarkers in serum, urine and tissue explores new discoveries in cancer genomics to better identify aggressive versus indolent disease.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Bastian, P. J. et al. Insignificant prostate cancer and active surveillance: from definition to clinical implications. Eur. Urol. 55, 1321–1330 (2009).
Loeb, S. et al. Overdiagnosis and overtreatment of prostate cancer. Eur. Urol. 65, 1046–1055 (2014).
Mahal, B. A. et al. Use of active surveillance or watchful waiting for low-risk prostate cancer and management trends across risk groups in the United States, 2010–2015. JAMA 321, 704–706 (2019).
Matoso, A. & Epstein, J. I. Defining clinically significant prostate cancer on the basis of pathological findings. Histopathology 74, 135–145 (2019).
National Comprehensive Cancer Network. NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines®) for prostate cancer V.3.2020 (NCCN, 2020).
Komisarenko, M., Martin, L. J. & Finelli, A. Active surveillance review: contemporary selection criteria, follow-up, compliance and outcomes. Transl Androl. Urol. 7, 243–255 (2018).
Bokhorst, L. P. et al. A decade of active surveillance in the PRIAS study: an update and evaluation of the criteria used to recommend a switch to active treatment. Eur. Urol. 70, 954–960 (2016).
Ouzzane, A. et al. Magnetic resonance imaging targeted biopsy improves selection of patients considered for active surveillance for clinically low risk prostate cancer based on systematic biopsies. J. Urol. 194, 350–356 (2015).
Patel, H. D., Chalfin, H. J. & Carter, H. B. Improving prostate cancer screening and diagnosis: health policy and biomarkers beyond PSA. JAMA Oncol. 2, 867–868 (2016).
Epstein, J. I., Walsh, P. C., Carmichael, M. & Brendler, C. B. Pathologic and clinical findings to predict tumor extent of nonpalpable (stage T1c) prostate cancer. JAMA 271, 368–374 (1994).
Jeldres, C. et al. Validation of the contemporary Epstein criteria for insignificant prostate cancer in European men. Eur. Urol. 54, 1306–1313 (2008).
Bastian, P. J., Mangold, L. A., Epstein, J. I. & Partin, A. W. Characteristics of insignificant clinical T1c prostate tumors. A contemporary analysis. Cancer 101, 2001–2005 (2004).
Conti, S. L. et al. Pathological outcomes of candidates for active surveillance of prostate cancer. J. Urol. 181, 1628–1633 (2009).
Tosoian, J. J. et al. Tumor volume on biopsy of low risk prostate cancer managed with active surveillance. J. Urol. 199, 954–960 (2018).
Partin, A. W. et al. Clinical validation of an epigenetic assay to predict negative histopathological results in repeat prostate biopsies. J. Urol. 192, 1081–1087 (2014).
D’Amico, A. V. et al. Determinants of prostate cancer-specific survival after radiation therapy for patients with clinically localized prostate cancer. J. Clin. Oncol. 20, 4567–4573 (2002).
Ploussard, G. et al. Prospective evaluation of an extended 21-core biopsy scheme as initial prostate cancer diagnostic strategy. Eur. Urol. 65, 154–161 (2014).
Abouassaly, R., Lane, B. R. & Jones, J. S. Staging saturation biopsy in patients with prostate cancer on active surveillance protocol. Urology 71, 573–577 (2008).
Kryvenko, O. N., Carter, H. B., Trock, B. J. & Epstein, J. I. Biopsy criteria for determining appropriateness for active surveillance in the modern era. Urology 83, 869–874 (2014).
Patel, H. D. et al. Prostate specific antigen velocity risk count predicts biopsy reclassication for men with very low risk prostate cancer. J. Urol. 191, 629–637 (2014).
Su, Z. T. et al. Downgrading of grade group 2 intermediate-risk prostate cancer from biopsy to radical prostatectomy: comparison of outcomes and predictors to identify potential candidates for active surveillance. Cancer. 126, 1632–1639 (2020).
Eggener, S. E. et al. Predicting 15-year prostate cancer specific mortality after radical prostatectomy. J. Urol. 185, 869–875 (2011).
Patel, H. D., Tosoian, J. J., Carter, H. B. & Epstein, J. I. Adverse pathologic findings for men electing immediate radical prostatectomy: defining a favorable intermediate-risk group. JAMA Oncol. 4, 89–92 (2018).
Zumsteg, Z. S. et al. A new risk classification for therapeutic decision making with intermediate-risk prostate cancer patients undergoing dose-escalated external-beam radiation therapy. Eur. Urol. 64, 895–902 (2013).
Musunuru, H. B. et al. Active surveillance for intermediate risk prostate cancer: survival outcomes in the Sunnybrook experience. J. Urol. 196, 1651–1658 (2016).
Patel, H. D. et al. Subtyping the risk of intermediate risk prosate cancer for active surveillance based on adverse pathology at radical prostatectomy. J. Urol. 200, 1068–1074 (2018).
Tosoian, J. J. et al. Intermediate and longer-term outcomes from a prospective active surveillance program for favorable risk prostate cancer. J. Clin. Oncol. 33, 3379–3385 (2015).
Huan, C. C. et al. Gleason score 3+4=7 prostate cancer with minimal quantity of Gleason pattern 4 on needle biopsy is associated with low-risk tumor in radical prostatectomy specimen. Am. J. Surg. Pathol. 38, 1096–1101 (2014).
Kir, G., Seneldir, H. & Gumus, E. Outcomes of Gleason score 3+4=7 prostate cancer with minimal amount <6% of Gleason pattern 4 tissue in needle biopsy specimens. Ann. Diagn. Pathol. 20, 48–51 (2016).
Kweldam, C. F. et al. Cribriform growth is highly predictive for postoperative metastasis and disease-specific death in Gleason score 7 prostate cancer. Mod. Pathol. 28, 457–464 (2015).
Kweldam, C. F. et al. Prostate cancer outcomes of men with biopsy Gleason score 6 and 7 without cribiform or intraductal carcinoma. Eur. J. Cancer 66, 26–33 (2016).
Lokman, U. et al. PTEN loss but not ERG expression in diagnostic biopsies is associated with increased risk of progression and adverse surgical findings in men with prostate cancer on active surveillance. Eur. Urol. Focus 4, 867–873 (2018).
Tosoian, J. J. et al. PTEN status assessment in the Johns Hopkins active surveillance cohort. Prostate Cancer Prostatic Dis. 22, 176–181 (2019).
Oberlin, D. T., Casalino, D. D., Miller, F. H. & Meeks, J. J. Dramatic increase in the utilization of mutliparametic magnetic resonance imaging for detection and management of prostate cancer. Abdom. Radiol. 42, 1255–1258 (2017).
Meng, M. V., Franks, J. H., Presti, J. C. Jr & Shinohara, K. The utility of apical anterior horn biopsies in prostate cancer detection. Urol. Oncol. 21, 361–365 (2003).
Lawrentschuk, N. et al. Prostatic evasive anterior tumors: the role of magnetic resonance imaging. BJU Int. 105, 1231–1236 (2010).
Scattoni, V. et al. Extended and saturation prostatic biopsy in the diagnosis and characterization of prostate cancer: a critical analysis of the literature. Eur. Urol. 52, 1309–1322 (2007).
Hu, J. C. et al. Targeted prostate biopsy to select men for active surveillance-do Epstein criteria still apply? J. Urol. 192, 385–390 (2014).
van As, N. J. et al. A study of diffusion-weighted magnetic resonance imaging in men with untreated localized prostate cancer on active surveillance. Eur. Urol. 56, 981–987 (2009).
Ahmed, H. U. et al. Diagnostic accuracy of multi-parametric MRI and TRUS biopsy in prostate cancer (PROMIS): a paired validating confirmatory study. Lancet 389, 815–822 (2017).
Kasivisvanathan, V. et al. MRI-targeted or standard biopsy for prostate-cancer diagnosis. N. Engl. J. Med. 378, 1767–1777 (2018).
Weinreb, J. C. et al. PI-RADS prostate imaging-report and data system: 2015, version 2. Eur. Urol. 69, 16–40 (2016).
Hofbauer, S. L. et al. Validation of prostate imaging reporting and data system version 2 for the detection of prostate cancer. J. Urol. 200, 767–773 (2018).
Pessoa, R. R. et al. Value of 3-Tesla multiparametric magnetic resonance imaging and targeted biopsy for improved risk stratification in patients considered for active surveillance. BJU Int. 119, 535–542 (2017).
Zhai, L. et al. The role of prostate imaging reporting and data system score in Gleason 3+3 active surveillance candidate enrollment: a diagnostic meta-analysis. Prostate Cancer Prostatic Dis. 22, 235–243 (2019).
Khoo, C. C. et al. Likert vs PI-RADS v2: a comparison of two radiological scoring systems for detection of clinically significant prostate cancer. BJU Int. 125, 49–55 (2020).
Amin, A. The magnetic resonance imaging in active surveillance “MRIAS” Trial: use of baseline multiparametric magnetic resonance imaging and saturation biopsy to reduce the frequency of surveillance prostate biopsies. J. Urol. 203, 910–917 (2020).
Klotz, L. et al. Randomized study of systematic biopsy versus magnetic resonance imaging and targeted and systematic biopsy in men on active surveillance (ASIST): 2-year post biopsy follow-up. Eur. Urol. 77, 311–317 (2020).
Gorin, M. A. et al. Prostate specific membrane antigen targeted 18F-DCFPyL positron emission tomography/computerized tomography for the preoperative staging of high-risk prostate cancer: results of a prospective, phase II, single center study. J. Urol. 199, 126–132 (2018).
Maurer, T., Eiber, M., Schqaiger, M. & Gschwend, J. E. Current use of PSMA-PET in prostate cancer management. Nat. Rev. Urol. 13, 226–235 (2016).
Loeb, S. & Tosoian, J. J. Biomarkers in active surveillance. Transl Androl. Urol. 7, 155–159 (2018).
Saini, S. PSA and beyond: alternative prostate cancer biomarkers. Cell Oncol. 39, 97–106 (2016).
de la Calle, C. et al. Multicenter evaluation of the prostate health index to detect aggressive prostate cancer in biopsy naïve men. J. Urol. 194, 65–72 (2015).
Houlgatte, A. et al. Use of [-2] pro PSA and phi index for early detection of prostate cancer: a prospective of 452 patients. Prog. Urol. 22, 279–283 (2012).
Fossati, N. et al. Preoperative prostate-specific antigen isoform p2PSA and its derivatives, %p2PSA and prostate health index, predict pathologic outcomes in patients undergoing radical prostatectomy for prostate cancer: results from a multicentric European prospective study. Eur. Urol. 68, 132–138 (2015).
Druskin, S. C. et al. Combining prostate health index density, magnetic resonance imaging and prior negative biopsy status to improve the detection of clinically significant prostate cancer. BJU Int. 121, 619–626 (2018).
Schwen, Z. R. et al. Prostate health index and multiparametric MRI to predict prostate cancer grade reclassification in active surveillance. BJU Int. 126, 373–378 (2020).
Punnen, S., Pavan, N. & Parekh, D. J. Finding the wolf in sheep’s clothing: the 4Kscore is a novel blood test that can accurately identify the risk of aggressive prostate cancer. Rev. Urol. 17, 3–13 (2015).
Zappala, S. M. et al. Clinical performance of the 4Kscore Test to predict high-grade prostate cancer at biopsy: a meta-analysis of us and European clinical validation study results. Rev. Urol. 19, 149–155 (2017).
Parekh, D. J. et al. A multi-institutional prospective trial in the USA confirms that the 4Kscore accurately identified men with high-grade prostate cancer. Eur. Urol. 68, 464–470 (2015).
Konety, B. et al. The 4Kscore test reduces prostate biopsy rates in community and academic urology practices. Rev. Urol. 17, 231–240 (2015).
Lin, D. W. et al. Evaluating the four kallikrein panel of the 4Kscore for prediction of high-grade prostate cancer in men in the canary prostate active surveillance study. Eur. Urol. 72, 448–454 (2017).
Sanda, M. G., Feng, Z. & Howard, D. H. Association between combined TMPRSS2:ERG and PCA3 RNA urinary testing and detection of aggressive prostate cancer. JAMA Oncol. 3, 1086–1093 (2017).
Lin, D. W. et al. Urinary TMPRSS2:ERG and PCA3 in an active surveillance cohort: results from a baseline analysis in the Canary Prostate Active Surveillance Study. Clin. Cancer Res. 19, 2442–2450 (2013).
Newcomb, L. F. et al. Performance of PCA3 and TMPRSS2:ERG urinary biomarkers in prediction of biopsy outcome in the Canary Prostate Active Surveillance Study (PASS). Prostate Cancer Prostatic Dis. 22, 438–445 (2019).
Tosoian, J. J. et al. Longitudinal assessment of urinary PCA3 for predicting prostate cancer grade reclassification in favorable-risk men during active surveillance. Prostate Cancer Prostatic Dis. 20, 339–342 (2017).
Van Neste, L. et al. Detection of high-grade prostate cancer using a urinary molecular biomarker-based risk score. Eur. Urol. 70, 740–748 (2016).
Mckiernan, J. et al. A novel urine exosome gene expression assay to predict high-grade prostate cancer at initial biopsy. JAMA Oncol. 2, 882–889 (2016).
McKiernan, J. et al. A prospective adaptive utility trial to validate performance of a novel urine exosome gene expression assay to predict high-grade prostate cancer in patients with prostate-specific antigen 2–10 ng/ml at initial biopsy. Eur. Urol. 74, 731–738 (2018).
Stewart, G. D. et al. Clinical utility of an epigenetic assay to detect occult prostate cancer in histopathologically negative biopsies: results of the MATLOC study. J. Urol. 189, 1110–1116 (2013).
Li, D., Kumaraswamy, E., Harian-Williams, L. M. & Jensen, R. A. The role of BRCA1 and BRCA2 in prostate cancer. Front. Biosci. 18, 1445–1459 (2013).
Sircar, K. et al. PTEN genomic deletion is associated with p-Akt and AR signaling in poorer outcome, hormone refractory prostate cancer. J. Pathol. 218, 505–513 (2009).
Shore, N. D. et al. Impact of the cell cycle progression test on physician and patient treatment selection for localized prostate cancer. J. Urol. 195, 612–618 (2016).
Cooperberg, M. R. et al. Validation of a cell-cycle progression gene panel to improve risk stratification in a contemporary prostatectomy cohort. J. Clin. Oncol. 31, 1428–1434 (2013).
Health Quality Ontario. Prolaris cell cycle progression test for localized prostate cancer: a health technology assessment. Ont. Health Technol. Assess. Ser. 17, 1–75 (2017).
Kaul, S. et al. Clinical outcomes in men with prostate cancer who selected active surveillance using a clinical cell cycle risk score. Per. Med. 16, 491–499 (2019).
Badani, K. K. et al. Effect of a genomic classifier test on clinical practice decisions for patients with high-risk prostate cancer after surgery. BJU Int. 115, 419–429 (2015).
Gore, J. L. et al. Decipher test impacts decision making among patients considering adjuvant and salvage treatment after radical prostatectomy: interim results from the multicenter prospective PRO-IMPACT study. Cancer 123, 2850–2859 (2017).
Herlemann, A. et al. Decipher identifies men with otherwise clinically favorable-intermediate risk disease who may not be good candidates for active surveillance. Prostate Cancer Prostatic Dis. 23, 136–143 (2020).
Klein, E. A. et al. A 17-gene assay to predict prostate cancer aggressiveness in the context of Gleason grade heterogeneity, tumor multifocality, and biopsy undersampling. Eur. Urol. 66, 550–560 (2014).
Lin, D. W. et al. 17-gene genomic prostate score test results in the canary prostate active surveillance study (PASS) cohort. J. Clin. Oncol. 38, 1549–1557 (2020).
Welty, C. J. et al. Extended follow p and risk factors for disease reclassification in a large active surveillance cohort for localized prostate cancer. J. Urol. 193, 807–811 (2015).
Adamy, A. et al. Role of prostate specific antigen and immediate confirmatory biopsy in predicting progression during active surveillance for low risk prostate cancer. J. Urol. 185, 477–482 (2011).
Soloway, M. S. et al. Active surveillance; a reasonable management alternative for patients with prostate cancer: the Miami experience. BJU Int. 101, 165–169 (2008).
Acknowledgements
The authors thank Yasin Bhanji and Alex J. Solomon for their contribution of MR images for this manuscript. Referenced with permission from the NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines®) for Prostate Cancer V.3.2020. © National Comprehensive Cancer Network, Inc. 201X. All rights reserved. Accessed January 14th 2020. To view the most recent and complete version of the guideline, go online to NCCN.org. NCCN makes no warranties of any kind whatsoever regarding their content, use or application and disclaims any responsibility for their application or use in any way.
Author information
Authors and Affiliations
Contributions
J.L.L., H.D.P., J.I.E. and A.W.P. researched data for the article, contributed to discussions of its content, wrote the manuscript and participated in review and/or editing of the manuscript before submission. N.M.H. additionally researched data for the article and contributed to discussions of its content.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Peer review information
Nature Reviews Urology thanks R. Valdagni, A. Finelli and C. Bangma for their contribution to the peer review of this work.
Permissions
Box 1 adapted with permission from the NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines®) for Prostate Cancer V.3.2020. © 2020 National Comprehensive Cancer Network, Inc. All rights reserved. The NCCN Guidelines® and illustrations herein may not be reproduced in any form for any purpose without the express written permission of NCCN. To view the most recent and complete version of the NCCN Guidelines, go online to NCCN.org. The NCCN Guidelines are a work in progress that may be refined as often as new significant data become available. NCCN makes no warranties of any kind whatsoever regarding their content, use or application and disclaims any responsibility for their application or use in any way.
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Glossary
- PSA
-
Prostate-specific antigen (PSA) is a glycoprotein enzyme that is prostate specific and one of the first serum tests developed in prostate cancer screening.
- PSA density
-
A calculation of total prostate-specific antigen (PSA) divided by prostate volume. This is helpful in interpreting clinical disease states.
- PSA kinetics
-
The absolute rate of prostate-specific antigen (PSA) change over time. This is helpful in interpreting clinical disease states.
- mpMRI fusion-targeted biopsy
-
A new approach using multi-parametric MRI (mpMRI) technology paired with guided prostate biopsy to provide a more accurate targeting approach.
- Total PSA
-
A blood test that measures the cumulative amount of prostate-specific antigen (PSA) in a patient.
- Free PSA
-
A blood test that measures the amount of PSA that is unbound to blood proteins and could be a helpful predictor in diagnosing prostate cancer.
Rights and permissions
About this article
Cite this article
Liu, J.L., Patel, H.D., Haney, N.M. et al. Advances in the selection of patients with prostate cancer for active surveillance. Nat Rev Urol 18, 197–208 (2021). https://doi.org/10.1038/s41585-021-00432-w
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41585-021-00432-w
This article is cited by
-
Prediction model of gleason score upgrading after radical prostatectomy based on a bayesian network
BMC Urology (2023)
-
Explainable ML models for a deeper insight on treatment decision for localized prostate cancer
Scientific Reports (2023)
-
Review of Active Surveillance in Underrepresented and High-Risk Populations: Feasibility and Safety
Current Urology Reports (2023)
-
The current role of MRI for guiding active surveillance in prostate cancer
Nature Reviews Urology (2022)
-
Adverse upgrading and/or upstaging in contemporary low-risk prostate cancer patients
International Urology and Nephrology (2022)