Abstract and Introduction
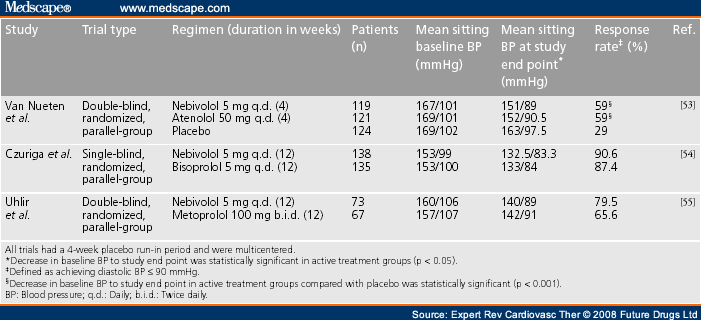
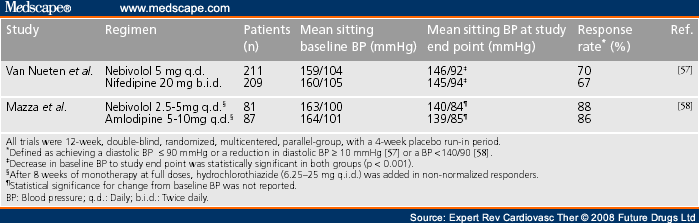
Hypertension is a major cardiovascular risk factor but most patients remain asymptomatic for many years. Successful therapy not only needs to be effective, it also needs to be well tolerated. β-blockers are well established as effective antihypertensive agents. However, one major drawback to the currently available β-blockers, particularly the noncardioselective β-blockers, is their side-effect profile, including sexual dysfunction, fatigue, depression and metabolic abnormalities such as impaired glucose tolerance and lipid abnormalities. Nebivolol (Bystolic®), a novel, highly cardioselective, third-generation β-blocker that recently received approval by the US FDA for the treatment of hypertension in the USA, is effective in treating blood pressure and has a favorable side-effect profile. Studies conducted in Europe, where nebivolol has been available for some time for the treatment of hypertension, have shown that nebivolol achieves blood pressure reductions comparable to other β-blockers but with fewer side effects. Additionally, nebivolol has demonstrated similar efficacy in blood pressure reduction when compared with calcium channel blockers and inhibitors of the renin–angiotensin system. When combined with hydrochlorothiazide there was an additive antihypertensive effect. Lastly, nebivolol exhibits a vasodilatory property that is related to its effect on nitric oxide, an intrinsic vasodilator produced in the vascular endothelium. Nebivolol enhances nitric oxide bioavailablility. Studies have also demonstrated nebivolol's ability to function as an antioxidant and decrease markers of oxidative stress. These effects are believed to ultimately produce a modulation of the endothelial dysfunction typically seen in hypertension.
Hypertension is a major contributor to cardiovascular disease and a leading cause of stroke, myocardial infarction, heart failure and kidney disease. It is estimated that more than 65 million Americans have hypertension[1] and its prevalence is expected to rise. The prevalence of hypertension increases with age and older patients are more likely to suffer from cardiovascular complications of hypertension. Although the benefits of hypertension treatment and control have been well documented, the majority of patients remain undertreated and poorly controlled.[2–5] In the USA, it has been estimated that less than 60% of patients receive any treatment and only 31% are adequately controlled.[2] Although multiple factors contribute to poor patient compliance, medication cost and side effects have frequently been blamed. Hypertension is an asymptomatic disease, and it is important to use effective and well-tolerated regimens as long-term therapy in order to maintain patient compliance.
Multiple medications have been approved for the treatment of hypertension, in general tabulated in one of six categories: diuretics, β-blockers, calcium channel blockers, blockers of the renin–angiotensin–aldosterone system, direct vasodilators and centrally acting agents. Each class of medication has a different mechanism of action and a potentially different side-effect profile. Most patients with hypertension require more than one agent to be controlled and it is logical to combine drugs with different mechanisms of action. The use of β-blockers is well established for the management of cardiovascular diseases,[6] and their ability to reduce cardiovascular complications has been shown in many patient populations. However, traditional noncardioselective β-blockers have been associated with side effects that often interfere with patient tolerability, such as decreased libido, erectile dysfunction, depression, fatigue, impaired glucose tolerance, insulin resistance and alterations in serum lipid levels.[7–9] Furthermore, trial data summarized in recent meta-analyses suggest that traditional β-blockers, particularly atenolol, may not be as effective as other classes of antihypertensive agents in preventing cardiovascular complications.[10,11]
Nebivolol is a novel β-blocker that has been available in Europe for a number of years for the treatment of hypertension and, more recently, for the treatment of congestive heart failure in elderly patients. Nebivolol (Bystolic®) was recently approved (December 2007) by the US FDA for the treatment of hypertension, either taken alone or in combination with other antihypertensive agents. Nebivolol is a third-generation β-blocker that exhibits highly selective β1-adrenergic receptor blockade and nitric oxide-mediated vasodilatation. The beneficial effects of nebivolol as an antihypertensive treatment are not associated with the usual side effects of other β-blockers.[12,13]
This article will review evidence from the published literature indicating that nebivolol is an effective and well-tolerated antihypertensive agent, with additional beneficial effects presumed to be related to its attenuation of oxidative stress, increase in nitric oxide levels and improvement of endothelial dysfunction.
Expert Rev Cardiovasc Ther. 2008;6(4):471-479. © 2008 Future Drugs Ltd.
/publishers/futdrug/erc/description/cover-erc.jpg
Cite this: Beta-blockers in the Management of Hypertension: Focus on Nebivolol - Medscape - Apr 01, 2008.










Comments