Equipment
Equipment required for suture closure of a wound includes the following:
-
Suture material
-
Needle
-
Needle holder
Suture material is a foreign body implanted into human tissues; consequently, it elicits a foreign-body tissue reaction. During wound closure, a sterile field and meticulous aseptic technique are critical to minimize the risk of wound infection. Other complications of wound healing, such as hypertrophic scars, wide scars, and wound dehiscence, may result from patient factors (eg, nutritional status), incorrect suture selection, or a technique that results in excessive tension across the wound.
Surgical needles are produced from stainless steel alloys, which have excellent resistance to corrosion. [28] All true stainless steels contain a minimum of 12% chromium, which allows a thin, protective surface layer of chromium oxide to form when the steel is exposed oxygen. Since their development during the early 1960s, high-nickel maraging stainless steels have found extensive use in structural materials in many applications that require a combination of high strength and toughness.
Wound closure and healing are affected by the initial tissue injury caused by needle penetration and subsequent suture passage. Needle selection, surface characteristics of the suture (eg, coefficient of friction), and suture-coating materials selected for wound closure are important factors that must be considered by the surgeon.
Suture qualities
The ideal suture material would have all of the following characteristics:
-
It is sterile
-
It is suitable for all purposes (ie, is composed of material that can be used in any surgical procedure)
-
It causes minimal tissue injury or tissue reaction (ie, is nonelectrolytic, noncapillary, nonallergenic, and noncarcinogenic)
-
It is easy to handle
-
It holds securely when knotted (ie, no fraying or cutting)
-
It has high tensile strength
-
It possesses a favorable absorption profile
-
It is resistant to infection
At present, unfortunately, no single material is available that can offer all of these characteristics. In different situations and in different areas of the body where tissue composition varies, different suture characteristics are required for adequate wound closure.
There are several fundamental and essential characteristics that all sutures should be manufactured to possess, as follows:
-
Sterility
-
Uniform diameter and size
-
Pliability for ease of handling and knot security
-
Uniform tensile strength by suture type and size
-
Freedom from irritants or impurities that would elicit tissue reaction
In addition, there are various characteristics of suture material that are described with the following terms:
-
Absorbable - Progressive loss of mass or volume of suture material; this does not correlate with initial tensile strength
-
Breaking strength - Limit of tensile strength at which suture failure occurs
-
Capillarity - Extent to which absorbed fluid is transferred along the suture
-
Elasticity - Measure of the ability of the material to regain its original form and length after deformation
-
Fluid absorption - Ability to take up fluid after immersion
-
Knot-pull tensile strength - Breaking strength of knotted suture material (10-40% weaker after deformation by knot placement)
-
Knot strength - Amount of force necessary to cause a knot to slip (this is related to the coefficient of static friction and plasticity of a given material)
-
Memory - Inherent capability of suture to return to or maintain its original gross shape (this is related to elasticity, plasticity, and diameter)
-
Nonabsorbable - Surgical suture material that is relatively unaffected by the biologic activities of the body tissues and is therefore permanent unless removed
-
Plasticity - Measure of the ability to deform without breaking and to maintain a new form after relief of the deforming force
-
Pliability - Ease of handling of suture material; ability to adjust knot tension and to secure knots (this is related to suture material, filament type, and diameter)
-
Straight-pull tensile strength - Linear breaking strength of suture material
-
Suture pullout value - Application of force to a loop of suture located where tissue failure occurs, which measures the strength of a particular tissue; this varies according to anatomic site and histologic composition (fat, 0.2 kg; muscle, 1.27 kg; skin, 1.82 kg; fascia, 3.77 kg)
-
Tensile strength - Measure of the ability of a material or tissue to resist deformation and breakage
-
Wound breaking strength - Limit of tensile strength of a healing wound at which separation of the wound edges occurs
Suture size refers to the diameter of the suture strand and is denoted by means of zeroes. The more zeroes characterizing a suture size, the smaller the resultant strand diameter (eg, 4-0 or 0000 is larger than 5-0 or 00000). The smaller the suture, the less the tensile strength of the strand.
Suture classification
Sutures may be classified in terms of their origin, their structure, and their absorbability.
Natural vs synthetic
Natural sutures can be made of collagen from mammal intestines or from synthetic collagen (polymers). Tissue reaction and suture antigenicity lead to inflammatory reactions, especially with natural materials. [29, 30] Synthetic sutures are made of artificial polymers.
Monofilament vs multifilament
Monofilament suture material is made of a single strand; this structure is relatively more resistant to harboring microorganisms. It also exhibits less resistance to passage through tissue than multifilament suture does. However, great care must be taken in handling and tying a monofilament suture, because crushing or crimping of the suture can nick or weaken it and lead to undesirable and premature suture failure.
Multifilament suture material is composed of several filaments twisted or braided together. It generally has greater tensile strength and better pliability and flexibility than monofilament suture material, and it handles and ties well. However, because multifilament materials have increased capillarity, the increased absorption of fluid may facilitate the introduction of pathogens, which increases the risk for wound infection and dehiscence.
Multifilament suture material is less stiff than monofilament suture material, but because the individual filaments of a multifilament suture are braided together, an increased coefficient of friction is created when the suture is passed through tissue. Multifilament sutures are often treated with special coatings to facilitate tissue passage and reduce subsequent tissue damage.
Absorbable vs nonabsorbable
Absorbable sutures provide temporary wound support until the wound heals well enough to withstand normal stress. Absorption occurs by enzymatic degradation in natural materials and by hydrolysis in synthetic materials. Hydrolysis causes less tissue reaction than enzymatic degradation.
The first stage of absorption has a linear rate, lasting for several days to weeks. The second stage is characterized by loss of suture mass and overlaps the first stage. Loss of suture mass occurs as a result of leukocytic cellular responses that remove cellular debris and suture material from the line of tissue approximation. Chemical treatments, such as chromic salts, lengthen the absorption time.
It is important to note that loss of tensile strength and the rate of absorption are separate phenomena. The surgeon must recognize that accelerated absorption may occur in patients with fever, infection, or protein deficiency, and this may lead to an excessively rapid decline in tensile strength. Accelerated absorption may also occur in a body cavity that is moist or filled with fluid or if sutures become wet or moist during handling before implantation.
Nonabsorbable sutures elicit a tissue reaction that results in encapsulation of the suture material by fibroblasts. The United States Pharmacopeia (USP) classification of nonabsorbable sutures is as follows:
-
Class I - Silk or synthetic fibers of monofilament, twisted, or braided construction
-
Class II - Cotton or linen fibers or coated natural or synthetic fibers in which the coating contributes to suture thickness without adding strength
-
Class III - Metal wire of monofilament or multifilament construction
Suture characteristics
Both absorbable and nonabsorbable surgical sutures can be made from either natural or synthetic polymers.
Absorbable natural sutures
Absorbable natural suture materials include the following:
-
Collagen
-
Plain surgical gut
-
Fast-absorbing surgical gut
-
Chromic surgical gut
Collagen sutures are derived from the submucosal layer of ovine small intestine or the serosal layer of the bovine small intestine. This collagenous tissue is treated with an aldehyde solution, which crosslinks and strengthens the suture and makes it more resistant to enzymatic degradation. Suture materials treated in this way are called plain gut.
The tensile strength of plain surgical gut is maintained for 7-10 days after implantation (this varies with individual patient characteristics), and absorption is complete within 70 days. This type of suture is used for (1) repair of rapidly healing tissues that require minimal support and (2) ligation of superficial blood vessels.
Fast-absorbing surgical gut is indicated for epidermal use (it is required only for 5-7 days) and is not recommended for internal use. A 2019 randomized evaluator-blinded split-wound comparative effectiveness trial found that for linear repair of cutaneous wounds, use of 6-0 fast-absorbing gut did not produce statistically significant differences in cosmetic outcomes, scar width, or incidence of complications. [31]
Chromic surgical gut is treated with chromium salt, which slows down the absorption rate (reaching complete absorption at 90 days). Tensile strength is maintained for 10-14 days. Tissue reaction is due to the noncollagenous material present in these sutures. In addition, patient factors affect absorption rates and make tensile strength somewhat unpredictable. Salthouse et al demonstrated that the mechanism by which chromic surgical gut reabsorbs is the result of sequential attacks by lysosomal enzymes. [32]
Natural-fiber absorbable sutures have several distinct disadvantages. First, they tend to fray during knot construction. Second, there is considerably more variability in their retention of tensile strength than is found with the synthetic absorbable sutures. A search for a synthetic substitute for collagen sutures began in the 1960s. Soon, procedures were perfected for the synthesis of high-molecular-weight polyglycolic acid, which led to the development of the polyglycolic acid sutures. [32]
Absorbable synthetic sutures
Absorbable synthetic sutures are composed of chemical polymers that are absorbed by hydrolysis and cause a lesser degree of tissue reaction after placement. Depending on the anatomic site, surgeon’s preference, and the required suture characteristics, the following types of synthetic absorbable suture may be considered including (but not limited to) the following:
-
Polyglactin 910 (Vicryl)
-
Polycaprolate (Dexon II)
-
Poliglecaprone 25 (Monocryl)
-
Polysorb
-
Polydioxanone (PDS II)
-
Polytrimethylene carbonate (Maxon)
-
V-Loc
-
Polyglytone 621 (Caprosyn)
Polyglactin 910 suture is a braided multifilament suture coated with a copolymer of lactide and glycolide (polyglactin 370). The water-repelling quality of lactide slows loss of tensile strength, and the bulkiness of lactide leads to rapid absorption of suture mass once tensile strength is lost. The suture is also coated with calcium stearate, which permits easy tissue passage, precise knot placement, and smooth tiedown.
The tensile strength pf polyglactin 910 suture is approximately 65% at day 14 after implantation. Absorption is minimal for 40 days and complete in 56-70 days. These sutures cause only minimal tissue reaction. These sutures are used in general soft-tissue approximation and vessel ligation.
A similar suture material is made from polyglycolic acid and coated with polycaprolate (Dexon II). This material is comparable to polyglactin 910 with respect to tensile strength and absorption profile.
Poliglecaprone 25 suture is a monofilament suture that is a copolymer of glycolide and ε-caprolactone. The suture has superior pliability, leading to ease in handling and tying. Tensile strength is high initially, 50-60% at day 7 after implantation, and is lost at day 21. Absorption is complete at 91-119 days. Poliglecaprone 25 sutures are used for subcuticular closure and soft-tissue approximations and ligations. A recent study by Regan et al reported that poliglecaprone 25 sutures caused significantly less suture extrusion than polyglactin 910. [33]
Polysorb is a braided absorbable suture produced from a Lactomer copolymer formed via synthesis of copolymers of glycolide and lactide (in a ratio of 9 to 1). The glycolide and lactide behave differently when exposed to tissue hydrolysis. Glycolide provides for high initial tensile strength but hydrolyzes rapidly in tissue. [23] Lactide has a slower and controlled rate of hydrolysis, or tensile strength loss, and provides for prolonged tensile strength in tissue.
To decrease their friction coefficient, the surfaces of Polysorb sutures are coated with an absorbable mixture of caprolactone-glycolide copolymer and calcium stearyl lactylate. [34] At day 14 after implantation, nearly 80% of the USP tensile strength of these braided sutures remains. Approximately 30% of their USP tensile strength is retained at day 21. Absorption is essentially complete between days 56 and 70.
Polydioxanone, a polyester monofilament suture, provides extended wound support and elicits only a slight tissue reaction. Tensile strength is 70% at day 14 and 25% at day 42. Wound support remains for up to 6 weeks. Absorption is minimal for the first 90 days and essentially complete within 6 months. Like other monofilament sutures, polydioxanone has a low affinity for microorganisms. It is used for soft-tissue approximation, especially in pediatric, cardiovascular, gynecologic, ophthalmic, plastic, and digestive (colonic) situations.
Polytrimethylene carbonate is similar to polydioxanone with regard to tensile strength and absorption profile.
V-Loc is a barbed suture manufactured from 0 polydioxanone that is self-anchoring, with no knots required for wound closure. The elimination of knot tying may reduce many of the challenges of knot construction. This suture consists of axially barbed segments on each side of a midpoint, at which the barbs change direction. The tensile strength of the barbed suture decreases over time. Each suture is attached to a premium cutting and taper-point needle with NuCoat coating technology. [35]
Caprosyn is rapidly absorbing and represents the most recent innovation in the development of monofilament absorbable synthetic sutures. Caprosyn sutures are prepared from polyglytone 621, which is composed of glycolide, caprolactone, trimethylene carbonate, and lactide. Implantation studies in animals indicate that Caprosyn suture retains a minimum of 50-60% USP knot strength at day 5 after implantation and a minimum of 20-30% of knot strength at day 10 days. All of its tensile strength is essentially lost by day 21.
Nonabsorbable natural sutures
Natural nonabsorbable sutures include the following:
-
Surgical silk
-
Surgical cotton
-
Surgical steel
Surgical silk is made of raw silk spun by silkworms. It may be coated with beeswax or silicone. Many surgeons consider silk suture the standard of performance because of its superior handling characteristics. Although classified as nonabsorbable, silk is absorbed by proteolysis and is often undetectable in the wound site by 2 years. Tensile strength decreases with moisture absorption and is lost by 1 year. The main problem with silk suture is the acute inflammatory reaction it triggers. Host reaction leads to encapsulation by fibrous connective tissue.
Surgical cotton is made of twisted, long, staple cotton fibers. Tensile strength is 50% within 6 months and 30-40% by 2 years. Surgical cotton is nonabsorbable and becomes encapsulated within body tissues.
Surgical steel suture is made of stainless steel (iron-chromium-nickel-molybdenum alloy) as a monofilament or a twisted multifilament. This suture can be made with flexibility, fine size, and the absence of toxic elements. Surgical steel demonstrates high tensile strength with little loss over time and low tissue reactivity. The material also holds knots well.
Surgical steel suture is used primarily in orthopedic, neurosurgical, and thoracic applications. This type of suture may also be used in abdominal wall closure, sternum closure, and retention. However, it can be difficult to handle because of kinking, fragmentation, and barbing, which render the wire useless and may present a risk to the surgeon’s safety. [36]
The cutting, tearing, or pulling of other patient tissues is also a risk. In addition, surgical steel in the presence of other metals or alloys may cause electrolytic reactions; therefore, it is not a safe choice in these circumstances. The size of a steel suture is classified according to the Brown and Sharpe gauge –that is, from 18 gauge (largest diameter) to 40 gauge (smallest diameter). The standard USP classification is also used to denote wire diameter.
Nonabsorbable synthetic sutures
Nonabsorbable synthetic sutures include the following:
-
Nylon (Ethilon/Monosof [monofilament] and Nurolon/Surgilon [braided])
-
Polyester fiber (Mersilene/Surgidac [uncoated] and Ethibond/Ti-cron [coated])
-
Polybutester (Novafil)
-
Coated polybutester (Vascufil)
-
Polypropylene (Prolene)
-
Surgipro II
Nylon is a polyamide polymer suture material available in monofilament and braided forms. Its elasticity makes it useful in retention and skin closure. Nylon is quite pliable, especially when moist. (A premoistened form is available for cosmetic plastic surgery.) The braided forms are coated with silicone. Nylon suture has good handling characteristics, though its memory tends to return the material to its original straight form.
Nylon has 81% tensile strength at 1 year after implantation, 72% at 2 years, and 66% at 11 years. It is stronger than silk and, unlike silk, elicits only a minimal acute inflammatory reaction. Nylon is hydrolyzed slowly, but the remaining suture material is stable at 2 years, as a consequence of gradual encapsulation by fibrous connective tissue.
Polyester fiber (Mersilene/Surgidac [uncoated] and Ethibond/Ti-cron [coated]) suture material, formed from a polymer of polyethylene terephthalate, is available either uncoated or coated with polybutilate or silicone. The coating reduces friction for ease of tissue passage and improved suture pliability and tiedown.
Polyester fiber sutures elicit minimal tissue reaction and last indefinitely in the body. they are stronger than natural-fiber sutures and do not weaken with moistening. The material provides precise, consistent suture tension and retains tensile strength. This suture is commonly used for vessel anastomosis and the placement of prosthetic materials.
Polybutester suture, composed of a block copolymer containing butylene terephthalate and polytetramethylene ether glycol, is a monofilament suture with unique performance characteristics that may be advantageous for wound closure. [37] With a polybutester suture, low forces yield significantly greater elongation than is seen in the other sutures. In addition, the elasticity of polybutester suture is superior to that of the other sutures, allowing the suture to return to its original length once the load is removed.
Coated polybutester suture is a unique absorbable polymer that enhances the clinical performance of polybutester suture by virtue of its coating, a polytribolate polymer composed of glycolide, ε-caprolactone, and poloxamer 188. [38] Coating the polybutester suture markedly reduces its drag force in musculoaponeurotic, colonic, and vascular tissue.
Polypropylene is a monofilament suture that is an isostatic crystalline stereoisomer of a linear propylene polymer, permitting little or no saturation. It does not adhere to tissues and is useful as a pullout suture (eg, in subcuticular closure). It also holds knots better than other monofilament synthetic materials do.
Polypropylene is biologically inert and elicits minimal tissue reaction. It is not subject to degradation or weakening and maintains tensile strength for up to 2 years. This material is useful in contaminated and infected wounds, minimizing later sinus formation and suture extrusion. Interestingly, a recent study compared poliglecaprone 25 with polypropylene for superficial closures and did not find a statistically significant difference in cosmetic results. [39]
Surgipro II is a polypropylene suture that was developed to have increased resistance to fraying during knot rundown, especially with smaller-diameter sutures. This material is extremely inert in tissue and has been found to retain tensile strength in tissues for as long as 2 years. Surgipro II is widely used in plastic, cardiovascular, general, and orthopedic surgery. It exhibits a lower drag coefficient in tissue than nylon does, making it ideal for use in continuous suture closure. [28]
Needle qualities
The ideal surgical needle would have the following characteristics:
-
It is made of high-quality stainless steel
-
It has the smallest diameter possible
-
It is stable in the grasp of the needle holder
-
It is capable of implanting suture material through tissue with minimal trauma
-
It is sharp enough to penetrate tissue with minimal resistance
-
It is sterile and corrosion-resistant to prevent introduction of microorganisms or foreign materials into the wound
The following terms are employed to describe various characteristics related to needle performance:
-
Strength - Resistance to deformation during repeated passes through tissue (ie, increased needle strength results in decreased tissue trauma); ultimate moment is the measure of maximum strength determined by bending the needle to 90°, and surgical-yield moment is the amount of angular deformation that can occur before permanent needle deformation results
-
Ductility - Resistance (of a needle) to breakage under a given amount of deformation or bending
-
Sharpness - Measure of the ability of the needle to penetrate tissue; factors affecting sharpness include the angle of the point and the taper ratio (ie, ratio of taper length to needle diameter)
-
Clamping moment - Stability of a needle in a needle holder, determined by measuring the interaction of the needle body with the jaws of the needle holder
Needle construction
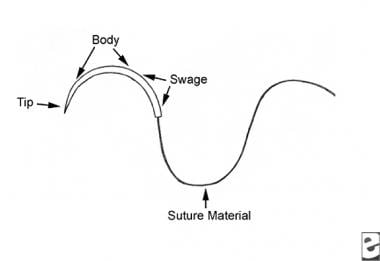
A surgical needle has three sections: the point, the body, and the swage (see the image below). The point is the sharpest portion and is used to penetrate the tissue. The body represents the midportion of the needle. The swage is the thickest portion of the needle and the portion to which the suture material is attached.
Point
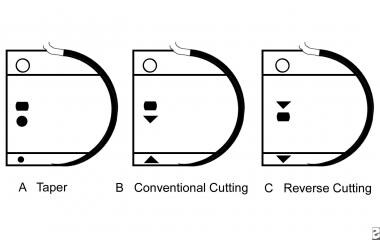
The point portion of the needle extends from the tip to the maximum cross-section of the body. Point types include the following (see the image below):
-
Cutting needles (conventional, reverse, or side [spatula])
-
Taper-point (round) needles
-
Beveled conventional cutting edge needles
A cutting needle has at least two opposing cutting edges (the point is usually triangular). This type is designed to penetrate dense, irregular, and relatively thick tissues. The point cuts a pathway through tissue and is ideal for skin sutures. Sharpness is due to the cutting edges.
Conventional cutting needles have three cutting edges (a triangular cross-section that changes to a flattened body). The third cutting edge is on the inner, concave curvature (surface-seeking).
In reverse-cutting needles, the third cutting edge is on the outer convex curvature of the needle (depth-seeking). These needles are stronger than conventional cutting needles and have a reduced risk of cutting out tissue. They are designed for tissue that is tough to penetrate (eg, skin, tendon sheaths, or oral mucosa). Reverse-cutting needles are also beneficial in cosmetic and ophthalmic surgery, causing minimal trauma.
Side-cutting (spatula) needles are flat on the top and bottom surfaces to reduce tissue injury. These needles allow maximum ease of penetration and control as they pass between and through tissue layers. Side-cutting needles were designed initially for ophthalmic procedures.
Taper-point (round) needles penetrate and pass through tissues by stretching without cutting. A sharp tip at the point flattens to an oval or rectangular shape. The sharpness is determined by the taper ratio (8-12:1) and the tip angle (20-35°). The needle is sharper if it has a higher taper ratio and a lower tip angle. The taper-point needle is used for easily penetrated tissues (eg, subcutaneous layers, dura, peritoneum, and abdominal viscera) and minimizes the potential tearing of fascia.
A beveled conventional cutting needle was developed with performance characteristics superior to those of other conventional cutting needles. It is composed of a unique stainless steel, ASTM 45500, that is heat-treated after the curving process to enhance its resistance to bending. The angle of presentation of the cutting edge is decreased to enhance sharpness. On the basis of the results of experimental and clinical studies done by Kaulbach et al, this beveled conventional cutting needle is recommended for closure of lacerations. [40]
Blunt point needles dissect friable tissue rather than cut it. The points are rounded and blunt, ideal for suturing the liver and kidneys. Additionally, blunt needles are being developed for more conventional uses in an effort to reduce needlestick injuries.
Body
Needle body types include the following:
-
Straight body
-
Half-curved ski body
-
Curved body
-
Compound curved body
The body part of the needle incorporates most of the needle length and is important for interaction with the needle holder and the ability to transmit the penetrating force to the point. Needle factors that affect this interaction include needle diameter and radius, body geometry, and stainless steel alloy. These components determine the needle-bending moment, the ultimate moment, the surgical-yield moment, and needle ductility.
The straight-body needle is used to suture easily accessible tissue that can be manipulated directly by hand. It is also used in microsurgery for nerve and vessel repair. Examples of straight-body needles include the Keith needle, which is used for skin closure of abdominal wounds, and the Bunnell needle, which is used for tendon and gastrointestinal (GI) tract repair.
The half-curved ski needle is rarely used in skin closure, because of its handling characteristics. The straight portion of the body does not follow the curved point, resulting in an enlarged curved point that makes the needle difficult to handle.
The curved needle has a predictable path through tissue and requires less space for maneuvering than a straight needle does. The semicircular path is the optimal course for sutures through tissue and provides an even distribution of tension. Body curvature commonly follows a 0.25-in., 0.375-in., 0.5-in., or 0.625-in. circle. The 0.375-in. circle is used most commonly for skin closure; the 0.5-in. circle was designed for confined spaces, and more manipulation (ie, increased wrist motion) by the surgeon is required.
The compound curved needle was originally designed for anterior-segment ophthalmic surgery. The body has a tight 80° curvature at the tip, which becomes a 45° curvature throughout the remainder of the body. A microvascular compound curved needle may also facilitate vessel approximation in microvascular surgery.
Swage
The suture attachment end creates a single, continuous unit of suture and needle, known as the swage. The swage may be designed to permit easy release of the needle and suture material (popoff) and includes the following types:
-
Channel swage
-
Drill swage
-
Nonswaged
In a channel swage, a needle is created with a channel into which the suture is introduced, and the channel is crimped over the suture to secure it into place. The diameter of the channel swage is greater than the diameter of the needle body.
In a drill swage, material is removed from the needle end (sometimes with a laser), and the needle is crimped over the suture. The diameter of the drill swage is less than the diameter of the needle body.
Alternatively, in a nonswaged needle, the suture may be passed through an eye, similar to that found in a sewing needle. In a closed-eye configuration, the shape may be round, oblong, or square. In a French (split or spring) eye, a slit is made in the end of the needle with ridges that catch and hold the suture in place.
Several disadvantages are associated with the use of a nonswaged needle. Passage of a double strand of suture through tissue leads to more tissue trauma. The suture is more likely to become unthreaded prematurely than it would be with a swaged needle. Moreover, decreased handling helps maintain suture integrity. Swaged sutures are not subject to suture fraying or damage caused by sharp corners in the eye of eyed needles.
Coating
The needle may be coated with silicone to permit easier tissue passage. The coating helps reduce the force needed to make initial tissue penetration and decrease the frictional forces as the body of the needle passes through the tissue.
Measurements
The chord length, or bite width, is the linear distance from the point of the curved needle to the swage (see the image below); the needle length is the distance measured along the needle from the point to the swage. The needle length, not the chord length, is the measurement supplied on suture packages. The radius, or bite depth, is the distance from the body of the needle to the center of the circle along which the needle curves; the diameter is considered the gauge or thickness of the needle wire.
Needle–needle holder interaction
The stability of the needle within the needle holder affects needle control and performance. The jaws of the needle holder must be appropriate to the needle size to hold it securely and prevent rocking, turning, and twisting (see the image below). An ovoid cross-section of the needle body often maximizes both the surface contact with the needle-holder jaws and the bending moment of the needle.
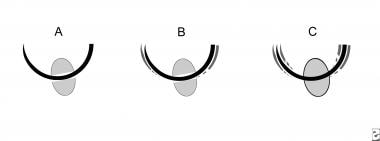 Interaction between needle holder and suture needle. (A) Needle holder of appropriate size for needle. (B) Needle holder that is too large for needle—pressure applied by needle holder leads to inadvertent straightening of suture needle. (C) Needle holder that is too small for needle—needle rotates around long axis of needle holder.
Interaction between needle holder and suture needle. (A) Needle holder of appropriate size for needle. (B) Needle holder that is too large for needle—pressure applied by needle holder leads to inadvertent straightening of suture needle. (C) Needle holder that is too small for needle—needle rotates around long axis of needle holder.
The needle-holder handle must be appropriate for the required depth of suture placement. The difference between the length of the handle and the jaw creates a mechanical advantage for exerting force through the needle point.
The needle-holder clamping moment is the force applied to a suture needle by a needle holder. The jaws of the needle holder contact a curved needle at one point on the outer curvature and at two points along the inner curvature. The force against the needle creates a moment arm, which acts to flatten the curvature of the needle.
Technically speaking, the needle-holder clamping moment must be less than the surgical yield of the needle, or the needle will bend and ultimately may break. A bent needle takes a relatively traumatic path through soft tissue and may cause increased soft-tissue injury. Repetitive injury by the needle holder also may cause the needle to break. If the broken portion of the needle is not identified and retrieved immediately, surgery may be delayed in an effort to find it. The need for intraoperative radiology and other potential difficulties may ensue.
Studies by Abidin et al demonstrated that the sharp edges of smooth needle-holder jaws cut the smooth surface of monofilament sutures, weakening their strength. [41] When the smooth tungsten carbide inserts of needle holders clamped 6-0 monofilament nylon suture with the first opposing teeth of the needle holder ratchet mechanism interlock, there was a significant reduction in suture breaking strength.
This damage to the suture can be prevented by mechanically grinding the outer edges of the smooth tungsten carbide inserts so as to achieve a rounded edge. When this was done, clamping the suture with the smooth jaws of the needle holder was atraumatic, with no demonstrable damage to the suture’s breaking strength. [41]
Monitoring and Follow-up
Suture removal
Sutures should be removed within 1-2 weeks of their placement, depending on the anatomic location. Prompt removal reduces the risk of suture marks, infection, and tissue reaction. The average wound usually achieves approximately 8% of its expected tensile strength 1-2 weeks after surgery. To prevent dehiscence and spread of the scar, sutures should not be removed too soon.
In general, the greater the tension across a wound, the longer the sutures should remain in place. As a guide, on the face, sutures should be removed in 5-7 days; on the neck, 7 days; on the scalp, 10 days; on the trunk and upper extremities, 10-14 days; and on the lower extremities, 14-21 days. Sutures in wounds under greater tension may have to be left in place slightly longer. Buried sutures, which are placed with absorbable suture material, are left in place because they dissolve.
Proper suture removal technique is essential for maintaining good results after sutures are properly selected and executed. Sutures are gently elevated with forceps, and one side of the suture is cut. The suture is then gently grasped by the knot and gently pulled toward the wound or suture line until the suture material is completely removed. If the suture is pulled away from the suture line, the wound edges may separate. Steri-Strips may be applied with a tissue adhesive to provide continued supplemental wound support after the sutures are removed.
-
Diagram of a needle.
-
Needle is placed vertically and longitudinally perpendicular to needle holder.
-
Needle holder is held through loops between thumb and fourth finger, and index finger rests on fulcrum of instrument.
-
Needle holder is held in palm, allowing greater dexterity.
-
Knot tying.
-
Simple interrupted suture placement. Bottom right image shows a flask-shaped stitch, which maximizes eversion.
-
Line of interrupted sutures.
-
Running suture line.
-
Running locked suture.
-
Vertical mattress suture.
-
Pulley stitch, type 1.
-
Far-near near-far modification of vertical mattress suture, creating pulley effect.
-
Horizontal mattress suture.
-
Half-buried horizontal suture (tip stitch, three-point corner stitch).
-
Subcuticular stitch. Skin surface remains intact along length of suture line.
-
Anatomy of needle.
-
Commonly used suture needles, with cross-sections of needles shown at point, body, and swage. (A) Taper-point needle. (B) Conventional cutting needle. (C) Reverse cutting needle.
-
Interaction between needle holder and suture needle. (A) Needle holder of appropriate size for needle. (B) Needle holder that is too large for needle—pressure applied by needle holder leads to inadvertent straightening of suture needle. (C) Needle holder that is too small for needle—needle rotates around long axis of needle holder.
-
Poster for Biogel Puncture Indication System.