By replacing microplates with microelectronics, researchers hope to make real-time diagnosis a reality. Disposable arrays that incorporate thousands of electronic sensors connected to signal processing circuitry could “help facilitate a new era of personalized medicine,” says John McDonald, chief research scientist at the Ovarian Cancer Institute in Atlanta and a professor in the Georgia Tech School of Biology.
October 27, 2010
|
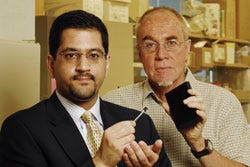
Associate professor Muhannad Bakir (left) holds a prototype electronic microplate, while professor John McDonald holds an example of the conventional microplate. |
Essentially, the technology would replace multiwelled microplates that have been used in biomedical research and diagnostic laboratories. These traditional devices test multiple samples for response to chemicals, organisms, and antibodies.
McDonald says that the devices using the microelectronics “could quickly detect in individuals the gene mutations that are indicative of cancer and then determine what would be the optimal treatment.” He says potential applications cannot be explored with current analytical and diagnostic technologies.
Fundamental to the new biosensing system is the ability to electronically detect markers that differentiate between healthy and diseased cells. These markers could be differences in proteins, mutations in DNA, or specific levels of ions that exist at different amounts in cancer cells. Researchers are finding that such minute differences could be exploited to create fast and inexpensive electronic detection techniques that don’t rely on conventional labels.
The Georgia Tech team’s goal is to create a sensing platform technology that uses nanoelectronics and 3-D electronic systems to aid microplates in detection and diagnosis. The 3-D sensor arrays are fabricated using conventional low-cost, top-down microelectronics technology. Although existing sample preparation and loading systems may have to be modified, the biosensor arrays should be compatible with existing work flows in research and diagnostic labs.
Separating the sensing and processing portions allows fabrication to be optimized for each type of device, notes Hyung Suk Yang, a graduate research assistant also working in the Nanotechnology Research Center. Without the separation, the types of materials and processes that can be used to fabricate the sensors are severely limited.
|
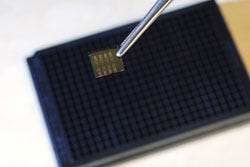
Shown above is an electronic microplate in front of the technology it aims to replace, the conventional microplate. |
So far, the researchers have demonstrated a biosensing system with silicon nanowire sensors in a 16-well device built on a 1 × 1-cm chip. The nanowires, measuring 50 × 70 nm, differentiated between ovarian cancer cells and healthy ovarian epithelial cells at a variety of cell densities.
Silicon nanowire sensor technology can be used to simultaneously detect large numbers of different cells and biomaterials without labels. The platform could accommodate a broad range of other sensors that may not have been invented yet. Ultimately, hundreds of thousands of different sensors could be included on each chip, enough to rapidly detect markers for a broad range of diseases.
Key features of the platform are that sensing is done using low-cost, disposable components, and information processing is done by reusable conventional integrated circuits connected temporarily to the array. Ultra-high-density springlike mechanically compliant connectors and through-silicon vias make the electrical connections while allowing technicians to replace the biosensor arrays without damaging the underlying circuitry.
The sensitivity of the tiny electronic sensors is potentially more efficient than current systems, thereby enabling earlier disease detection. Sample wells would be substantially smaller than those of current microplates—allowing a smaller form factor and more testing with a given sample volume.
Although many technical challenges remain, the ability to screen for thousands of disease markers in real time holds significant appeal. “With enough sensors in there, you could theoretically put all possible combinations on the array,” McDonald says. “This has not been considered possible until now because making an array large enough to detect them all with current technology is probably not feasible. But with microelectronics technology, you can easily include all the possible combinations, and that changes things.”
Papers describing the biosensing device were presented at the Electronic Components and Technology Conference and the International Interconnect Technology conference in June 2010. The research has been supported in part by the National Nanotechnology Infrastructure Network (NNIN), Georgia Tech’s Integrative BioSystems Institute (IBSI), and the Semiconductor Research Corp.
About the Author(s)
You May Also Like