PHOTO: Jeff and Lee Muth of Meiners Oaks. Photo submitted.
by Kimberly Rivers
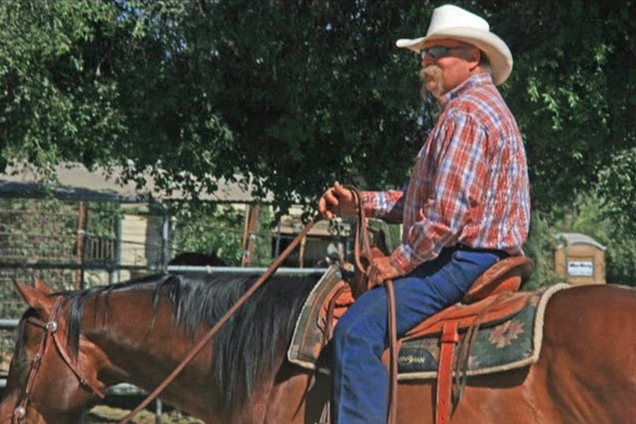
Lee Muth is upbeat and hopeful in sharing her and her husband’s harrowing story with COVID-19 that continues to unfold. They live in Meiners Oaks, with some horses and chickens. She works with the United States Postal Service (USPS) and Jeff is a fourth generation oil field worker.
She connected with the Ventura County Reporter on Monday, Jan. 11, after taking Jeff out for a walk. Today, Jeff requires her help due to the effects of a COVID-related stroke. They’ve been able to manage because of help from their friends and church community and Lee is hopeful that he’ll fully recover.
COVID, not a cold
On Nov. 30, 2020, Lee felt the onset of basic cold symptoms.
“I was sick with a chest cold on a Monday, I called my doctor on Tuesday,” she said. Lee had to get a note from her doctor to verify she was ill for her job at the USPS. “You don’t just call in sick, you need a note.” Her doctor wrote a note for her to stay home from work for the next week and she got tested that day. “I got a phone call on Friday . . . on Dec. 4, I found out I was positive.” Her doctor said she should let her husband know and he should also stay home from work. Jeff came home and got tested. It was positive.

Jeff Muth. Photo submitted.
They quarantined, and Lee began to feel better after two weeks with only a mild cough. Jeff got tested again 14 days later, and was still positive. Jeff is just 60 years old and Lee said he has no underlying health conditions. He had some chest pains in November and had a full cardiovascular work up, but the doctors said all was well.
About the second positive test, “According to two doctors that’s not terribly uncommon, sometimes it stays in your system,” Lee explained. The doctors told her they wouldn’t be able to retest her for two months, “maybe even 60 to 90 days, before a retest.”
After the two week quarantine and second positive test, Lee said that Jeff started to get sicker. “He got bronchitis, in his lungs . . . I rushed him to the ER on a Monday.”
He went to the emergency room at Ojai Valley Hospital, where doctors found scarring and inflammation in his lungs and prescribed Azithromycin, Dexamethasone and Virtussin, a cough syrup.
Back at home he was feeling dizzy now and then, “numbness and tingling on his right side.” Lee said everything Jeff was feeling was a stated side effect of the medication. As the tingling continued, the doctors said it was alright to stop the medications, that they’d “figure something else out.”
COVID-19 leads to stroke
Things took a turn for the worse that same night, when Jeff had a stroke.
According to Lee, as he was sitting on the couch, “his words started slurring, then he couldn’t move his right leg…I rushed him to the ER. He had a stroke more than likely from having COVID . . . it was a clot in his brain.”
According to the Mayo Clinic, COVID-19 can make blood cells more likely to clump up and form clots, which can lead to a stroke. At Ojai Valley Hospital, Jeff received tissue plasminogen activator treatment (tPA) — an intravenous injection of recombinant tissue plasminogen activator or alteplase. The treatment is designed to restore blood flow quickly by dissolving the clot causing the stroke.
Jeff stayed in the hospital for about four hours “on standby waiting to be cleared to be moved.” She said doctors told her one risk of the treatment is that someone may “bleed out if something happens,” such as a patient being moved too soon after treatment. Later, he was transported by ambulance to Community Memorial Hospital in Ventura and was immediately admitted to the intensive care unit.
“The whole time, I was not permitted to go in,” Lee said. “It was frustrating, sitting in a parking lot, scared for your husband.”
Jeff spent four days in the ICU, then was moved into a COVID-19 isolation room. In total he spent a week in the hospital. Lee said that everywhere Jeff was, he was “taken good care of,” and fully acknowledged the trying time hospital staff are experiencing. But the experience was difficult for both of them.
“That’s hard, having someone that is that ill and out of it, stuck in their own room,” said Lee. “He couldn’t answer his phone, he couldn’t remember the passcode,” and he couldn’t reach the hospital phone when Lee would call. “It was horrible, it was so hard. With COVID going on you can’t go in and sit with them, so they are alone…they need people to be there, to know someone is thinking about you,” wanting you to “hurry up and get well. Only four times a day someone would step in and that was it, take care of him and then leave. Horrible. These times are terrible, this COVID.”
The next morning Lee got a call that Jeff was not able to swallow or talk or move on the right side. Doctors told her his “brain did not know the right side existed, you need to be prepared, people don’t always come out of this.”
She reached out to her church. “Our prayer group, people that know and that love him. Prayers work . . . two days later he’s able to eat breakfast, move his arm and a little bit of his leg. The doctors don’t believe how much he’s progressed. God is good.”
COVID complicates recovery
From the hospital Jeff was moved to Victoria Care Center, a skilled nursing facility.
“They are extremely wonderful people,” said Lee.
Jeff was supposed to be there for 30 days, and receive extensive physical therapy. “When he got there, a majority of their staff got COVID and were under quarantine . . . So there was no one to help him to do physical therapy.”
At one point Jeff’s doctor was updated on the situation at the facility and, when reviewing Jeff’s chart, realized that beyond basic care, Jeff had essentially laid in bed for seven days. Lee doesn’t fault the care center at all; she saw them doing the best they could with an incredibly limited staff.
“I was amazed by them,” Lee said about the staff at Victoria Care Center. “They are in a tough situation with more than half [their staff] under quarantine, it’s a totally unprecedented circumstance.” She said they were as attentive as they could be, and kept her informed, emailing every morning “to give me a count” about the COVID levels among staff. “They were so up-front,” reporting “four more staff out today, under quarantine. That is pretty cool, they could have easily not said anything.”
But with the inability to provide physical therapy, Lee said “there is no way he could have stayed there.”
Considering the limits of care at Victoria, and at the doctors’ suggestion, Lee decided to move Jeff home. The care providers said they could send someone to their house to do physical therapy, while Lee could be with Jeff and care for him. That sounded ideal.
The reality, however, was much different.
“I have since found out that no one is willing to come to our house to do physical therapy,” Lee said. “He’s been tested three times and all three times tested positive for COVID. The doctors say he may not be contagious, but it is a big red flag.”

Lee and Jeff Muth. Photo submitted.
Despite this, under Lee’s care, Jeff is making good progress.
“His short-term memory is gone, he has incredible numbness and tingling, but he’s feeling more of it,” she explained. Every day Lee said that Jeff is able to tell her he’s “feeling better.”
“So we are doing it on our own. It’s been going OK. I’m not good at it. I’m trying, and he deserves it. I don’t want this to keep him from becoming himself again, he shouldn’t be denied that from any of this.”
While Lee said that now, more than a month after having COVID-19, she feels fine, she noted, “It’s weird though, my sense of smell is barely coming back. He doesn’t have smell or taste quite yet.”
Help from friends
As to how they are handling this, Lee admitted that it’s been “scary. We’ve had immense support from our church, bringing us dinner. They are going to the restaurants we like and are bringing us food at night.”
The support is desperately needed: After being diagnosed with cancer in 2015, Lee learned that her employer, USPS, didn’t have any option for disability pay in the event that employees get sick or need to leave work to care for a sick family member.
At the time of Lee’s diagnosis, “I thought I’d be OK.” Her doctors filled out the necessary forms for disability payments, but the paperwork “came back with zero, no way, you don’t receive it…We don’t have anything. If we’re out for any reason — sickness, disability, a family member needs help — it’s harder than heck to get help. We don’t have disability . . . you use up vacation, use up your sick days.”
This is the situation Lee finds herself in once again, now that she’s caring for Jeff.
Thankfully, however, the Muths have found help from their friends. Some started a GoFundMe campaign, and another set up an account at the local feed store, “so I can go get hay. I don’t have to worry about the horses or the chickens. It’s so humbling, that they care that much. It’s taken off such a load.”
Looking forward, Lee plans to go back to work next month, but she needs to know that Jeff can “care for himself. That he can take care of himself and be OK being by himself during the day . . . that is our goal.”
The GoFundMe campaign for the Muth family is online at www.gofundme.com/f/ojai-community-friends-need-our-help.
Information about COVID-19 and longterm effects is online at www.mayoclinic.org/diseases-conditions/coronavirus/in-depth/coronavirus-long-term-effects/art-20490351#:~:text=Even%20in%20young%20people%2C,that%20causes%20temporary%20paralysis.