Abstract
Literature on familial risk of carcinomas in situ (CISs) is limited because many cancer registries do not collect information on CIS. In Sweden CISs are collected, and we used these data to analyze familial relative risks (RRs) for concordant (CIS-CIS) types of anogenital (cervical, other female and male genital and anal) and skin squamous cell CIS; additionally RRs were assessed between CIS types and between CIS and invasive forms. RRs were calculated for the offspring generations when family members were diagnosed CIS. Case numbers for CIS ranged from 330 in anal to 177,285 in cervical CIS. Significant concordant CIS-CIS RRs were 2.74 for female genital, 1.77 for cervical and 2.29 for SCC skin CISs. The CIS forms associated also with each other, except for cervical and skin CIS types. RRs for concordant CIS-invasive cancer associations were lower than CIS-CIS associations. Cervical CIS associated with non-Hodgkin CIS which may suggest immune dysfunction as a contributing factors. The results for anogenital CIS types suggest that life style related human papilloma virus infections contributed to the observed familial associations. Lower risks for CIS-invasive cancer than CIS-CIS suggest that CIS and invasive cancers share only partially risk factors that underlie familial clustering.
Similar content being viewed by others
Introduction
Dysplasia is the earliest form of precancerous lesion and high-grade dysplasia is often synonymously referred to as carcinoma in situ (in situ cancer, CIS)1. CIS is a local accumulation of dysplastic cells. While CIS has not spread through its membranous borders, such as basement membrane, it may have the potential to do so and transform into cancer1,2. Because of cervical cancer screening programs, cervical CISs are very common and in many countries far outnumber invasive cervical cancers. Similarly, CIS for skin squamous cell (SCC) may outnumber the invasive SCCs in the skin3,4. Literature on CISs is limited because many cancer registries do not collect information on them. In Sweden, notifications of CISs to the cancer registry are mandated similar to invasive cancer, and these are included in the Swedish Family-Cancer Database5.
Considering that CIS may be a precursor stage to malignant tumors the risk factors may be shared and for many environmental risk factors this appears to be the case2. Data on relative risks for breast, melanoma and some other CISs in families of concordant invasive cancer suggest that familial risk for CIS may be approximately equal to familial risks between the invasive forms of these cancers but data on concordant CISs are limited6,7,8. In the present study we assess familial risks of anogenital (cervical, other female and male genital and anal) cancers and skin cancers between CISs types and between CIS and invasive forms in order to test the hypothesis of shared familial risk factors to be extended to CIS, for which data are lacking in many cancer registries. Our previous study on familial CIS published in 2008 included far lower case numbers (e.g., only ¼ for male genital and 1/3 for female genital CIS); furthermore, it was limited to genital cancers and the present inclusion of upper aerodigestive tract and colorectal cancers, melanoma and non-Hodgkin lymphoma is completely novel7. According to the International Classification of Diseases version 7, ‘other female genital cancers’ include the vulva and the vagina; ‘other male genital cancers’ include the penis and the scrotum. These CISs and cancers share the SCC histology9. Anogenital cancers are associated with human papillomavirus (HPV) infection, particularly related to the alpha genus of mucosal HPV types 16 and 1810,11. In skin SCC the beta genus HPVs may be playing a role but the evidence has not been equivocal12,13. Another common denominator for these cancers is increasing risk in cases of immunodeficiency14,15,16. The risk is high in immunosuppressed organ transplant patients13,14,15. As immune deficiency may be an important contributor even to cancers unrelated of infection, inclusion of non-Hodgkin lymphoma in the present study is relevant, as it is one of the most responsive cancers to immunosuppression14,16,17.
We use the Swedish Family-Cancer Database which is the largest family dataset in the world with a globally unique collection of CIS cases. We analyzed risks for both concordant (same cancer sites) and discordant (different cancer sites) CISs and also including invasive cancers of the cervix, other female genitals and skin. In order to internally confirm the results we assess familial risks bi-directionally (in reverse order) as explained in Methods. For parent-offspring relationships the bidirectional analyses are essentially independent and, when agreeing, such data would provide support for true biological associations.
Results
The RRs were calculated to the 0–83 year old offspring generation for with 303,630 CIS cases were reported to the cancer registry (Supplementary Table 1). The largest numbers were for cervical (177,285, median diagnostic age 32 years) and skin (36,516, 68 years) CISs. The number of CISs in the anus was 330, in other female genital it was 3326 and in other male genital it was 1000. Considering also the parental generation the total CIS numbers reached 464,484.
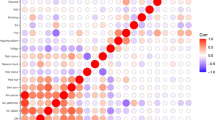
Risks for concordant sites are shown in Table 1 for familial CIS-CIS and CIS-invasive cancer associations. RRs were calculated for daughters whose first-degree family members were diagnosed with concordant CIS or invasive cancer. For cervical CIS, 20,188 familial patients were detected, resulting in RR of 1.77. The RR was 1.41 for invasive cervical cancer when a family member was diagnosed with cervical CIS; in reverse order the RR for cervical CIS was 1.54 when a family was diagnosed with invasive cervical cancer. Note that the differences between CIS-CIS and CIS-invasive cancer analyses were significant, i.e., 95% confidence interval (CIs) did not overlap. For other female genital cancer only CIS-CIS association of RR 2.74 was significant. For skin SCC the RR for CIS-CIS association was 2.29 which was significantly higher than both of the CIS-invasive associations (1.92 and 2.07). For skin cancer male and female risks did not differ.
Discordant associations of cervical CIS are shown in Table 2. Bi-directional associations for cervical CIS cancer were found for other female genital CIS (1.59 and 1.79) and non-Hodgkin lymphoma (1.24 and 1.36). Among CIS-invasive pairs none were bi-directionally significant but the risk for female genital CIS was increased (1.42) when a family member had invasive cervical cancer; for upper aerodigestive tract CIS the RR was 1.57 when a family member had invasive cervical cancer. The bottom line shows the RRs for all CISs or invasive cancers combined, with significant differences between respective CIS-CIS pairs and invasive-CIS pairs (1.35 vs. 1.12), and CIS-CIS pairs and CIS-invasive pairs (1.52 vs 1.31). When relevant, sex-specific risks were considered but none of the differences were significant (95%CIs overlapped).
In Table 3, discordant familial risks for other female genital CIS-CIS analyses showed increased bi-directional associations for cervical (RRs 1.79 and 1.59), skin (1.25 and 1.38), other male genital (2.82 and 3.79) and ovarian CIS (1.66 and 1.85). Among CIS-invasive pairs the only bidirectional association was noted with cervical cancer (1.48 and 1.19 which was significantly lower than 1.59 for the comparable CIS-CIS analysis). In the bottom line significant differences between respective combined CIS-CIS pairs and invasive-CIS pairs are shown (1.48 vs. 1.15), similar to CIS-CIS pairs and CIS-invasive pairs (1.46 vs 1.13). Sex-specific risks were not significant.
Similar discordant analyses were carried out with CIS and invasive SCC skin cancer (Table 4). Bi-directional CIS-CIS associations were observed with skin CIS and other female genital (1.38 and 1.25), upper aerodigestive tract (1.48 and 1.33), skin melanoma (1.63 and 1.59) CISs. The two latter ones showed also bi-directional associations in CIS-invasive pairs which however were of the same magnitude as the respective CIS-CIS associations. In contrast to the previous tables there was no significant difference between the combined CIS-CIS and CIS-invasive cancer RRs in the bottom line.
We carried out detailed analyses for two rare CIS types, other male genital and anal CIS but because of low case numbers no data are shown. The only significant bi-directional association was found with other female genital CIS; the RR for other male genital CIS was 3.79 (N = 6; 95%CI 1.70–8.46) when a family member was diagnosed with other female genital CIS, and it was 2.82 (N = 5; 95%CI 1.17–6.78) for female genital CIS when a family member was diagnosed with male genital CIS. For anal CIS-CIS pairs no bi-directional associations were found. Invasive anal cancer was associated with cervical CIS (RR 1.39; N = 131, 95%CI 1.16–1.66) and cervical CIS was associated with invasive anal cancer (RR 1.44; N = 327, 95%CI 1.29–1.60). Individual associations were found for anal CIS with male and female genital cancers and with non-Hodgkin lymphoma.
Discussion
In this systematic assessment of familial risks among CISs and between CIS and invasive anogenital and skin cancers several novel observations emerged. For three CISs we showed concordant bi-directional associations, including also associations between CIS and invasive cancer at the same sites. Additionally, we could define consistent clustering between CIS at discordant sites and some were even supported by associations with invasive cancers. It is likely that the clustering can be explained at least in part by shared HPV infections and/or deficiencies in host immune response to infections7.
The concordant risks for CIS were 2.74 for female genitals, 1.77 for cervical and 2.29 for SCC skin CISs. Risks for concordant association between CIS and invasive cancers were consistently lower than for concordant CIS-CIS associations. For other female genital cancer, CIS-invasive cancer associations were not significant but the case numbers were low. For cervical and skin sites, CIS-CIS associations were significantly higher than the respective CIS-invasive cancer associations (1.41 and 1.54, the bi-directional risk for cervical CIS-invasive; 1.92 and 2.07, the bi-directional risk for skin CIS-invasive). The low case numbers for other female genital cancers do not allow conclusions. On contrary, the large case numbers for cervical and skin CIS and invasive cancers suggest that the CIS and invasive types share familial risk factors to some degree but these appear not to be identical. These data appear consistent with the model that CIS may be a precursor of invasive cancer but the progressing clone of cells has acquired properties distinguishing them from the precursor population. For example, a clone of cells with specific HPV mutations will allow escape from host immune surveillance.
For comparison, in our recent analysis of invasive cancers, concordant other female genital cancers showed an RR of 2.72, almost exactly as the present CIC-CIS result of 2.74 (unpublished). According to the literature, for concordant invasive cervical cancer familial associations have been 1.80 (between sisters) and 1.74 (between daughter and mother)7. For invasive skin SCC concordant familial association has been reported as 2.0618.
Cervical CIS associated with female genital and anal CIS (and to some degree with invasive types) which would be consistent with susceptibility to HPV infections. Cervical CIS was also consistently associated with non-Hodgkin lymphoma. Based on cancers arising in immunosuppressed patients, non-Hodgkin lymphoma is considered one of the hallmarks of dysfunctional immune system14,15. Thus HPV susceptibility may be assisted by weak immune resistance shared by family members. HPV infections are usually sexually transmitted which would be unlikely to explain familial risk, and non-sexual transmissions from an infected mother during pregnancy or early childhood are supposed to be rare19,20. We assume that shared life-style with many sexual partners may the explanation to the observed familial risks. In our previous study on women who had children with different men in Sweden we observed increased risks for many life-style related cancers, including cervical, other female genital, upper aerodigestive tract, anal, liver, and lung cancers21. The results would thus suggest a gene-environment association in which immune dysfunction would be the genetic partner and HPV the environmental actor.
It is noteworthy that there was no association between cervical and skin CISs for which the infective HPV genus is suggested to be different and ultraviolet irradiation is the risk factor for skin SCC only12. The case numbers were large and the lacking of risk was consistent in Tables 2 and 4. Yet skin CIS was associated with female genital and upper aerodigestive tract CISs, both of which are known targets of mucosal HPV types12. The explanation remains unclear but the diagnostic age for skin CIS (68 years) was more than doubled for that of cervical CIS (32 years). A curious bi-directional association was noted between ovarian CIS and other female genital CIS. Previous data on the possible role of HPV in ovarian cancer is inconclusive, based on small positive and negative studies12.
In conclusion, the results showed that anogenital CISs showed concordant familial associations and discordant associations between each other, most likely related to a life-style with risk of HPV infections. For cervical CIS association with non-Hodgkin lymphoma CIS suggested contribution by immune dysfunction. Familial risks were lower for concordant CIS-invasive cancer associations than for CIS-CIS associations which suggests only a partial overlap of risk factors for the CIS and invasive cancers.
Methods
Database and cancer ascertainment
We used the update of the Swedish Family-Cancer Database which covered CIS and invasive cancers from 1958 through 2015 and family links over a century22. The Database includes 16 million individuals, covering the offspring generations born between 1932 and 2015 and their biological parents (the parental generation) in some 4 million nuclear families. Siblings could be identified only in the offspring generation which reached a maximal age of 83 years in 2015.
Coverage of cytologically or histologically verified incident cancers is considered to be over 90% complete on account of compulsory nationwide registration by clinicians and pathologists23. Cancer identification was based on the four-digit code according to the 7th revisions of the International Classification of Diseases (ICD-7).
Statistical analysis
Relative risks (RRs) were used to estimate cancer risks and each table contained three or four different but related analyses. RRs were calculated for the offspring generation. The first pair of data included CIS-CIS risks: (1) risk for CIS X when family members (parents of siblings) were diagnosed with any defined CIS, and (2) risk for any defined CIS and risk when family members were diagnosed with CIS X. For concordant CISs (Table 1) the results for (1) and (2) were identical and the data were not repeated. The second pair of data included invasive cancer-CIS: (3) risk for cancer X in offspring when family members were diagnosed with any defined CIS, and 4) risk of any defined CIS when family members were diagnosed with cancer X. Analyses (1) and (2) as well as (3) and (4) are independent for discordant cancers, and positive results in both analyses provided strong support for a true association. The differences between analyses (1) and (3), or (2) and (4) differ in that invasive cancer at the same site is replaced by CIS, and is being used to compare RRs between CIS-CIS and CIS-invasive associations.
Follow-up was started for each offspring at birth, immigration or January 1st, 1958, whichever came latest. Follow-up was terminated on diagnosis of CIS or invasive cancer, death, emigration, or the closing date of the study, which was December 31st, 2015. Termination of follow-up at diagnosis of the first tumor is a standard practice in cancer epidemiology to guard against biases such as surveillance bias24. The reference rates were generated for the same CIS or invasive cancer for those who did not have the relevant family history. Poisson regression modeling was employed to estimate RRs and corresponding 95% confidence intervals (CI). Potential confounders, including sex, age group (5-year bands), period (5-year bands), socioeconomic status (blue-collar worker, white-collar worker, farmer, private, professional, or other/unspecified) and residential area (large cities, South Sweden, North Sweden, or unspecified) were added to the model as covariates.
All statistical analyses were done with the SAS version 9.4. Data are shown in tables for anogenital (cervix, other female and male genital, upper aerodigestive tract) and skin CISs, for common CIS types (breast and colorectum) and for any bi-directional associations (ovary in Table 3).
Ethical statement
The study was approved by the Ethical Committee of Lund University (Reg.nr 2012/795), Sweden, and the study was conducted in accordance with the approved guidelines not requesting informed consent. The study is national register-based study on anonymous personal data.
References
Kumar, V., Cotran, R. & Robbins, S. Basic Pathology, 1–775 (W. B. Saunders, Philadelphia, 1997).
Voltaggio, L. et al. Current concepts in the diagnosis and pathobiology of intraepithelial neoplasia: A review by organ system. CA Cancer J Clin 66, 408–36 (2016).
Hussain, S. K., Sundquist, J. & Hemminki, K. Incidence trends of squamous cell and rare skin cancers in the Swedish national cancer registry point to calendar year and age-dependent increases. J Invest Dermatol 130, 1323–8 (2010).
Centre for Epidemiology. Cancer incidence in Sweden 2012, (The National Board of Health and Welfare, Stockholm, 2013).
Pukkala, E. et al. Nordic Cancer Registries - an overview of their procedures and data comparability. Acta Oncol 57, 440–55 (2018).
Chen, T. et al. Multiple primary (even in situ) melanomas in a patient pose significant risk to family members. Eur J Cancer 50, 2659–67 (2014).
Hussain, S. K., Sundquist, J. & Hemminki, K. Familial clustering of cancer at human papillomavirus-associated sites according to the Swedish Family-Cancer Database. Int J Cancer 122, 1873–8 (2008).
Lorenzo, B. J. & Hemminki, K. Familial risk of cancer shortly after diagnosis of the first familial tumor. J Natl Cancer Inst 97, 1575–9 (2005).
Tavassoli, F. & Devilee, P. (eds). Tumours of the breast and female genital organs, 432 (IARC Press, Lyon, 2003).
Zur Hausen, H. The search for infectious causes of human cancers: where and why. Virology 392, 1–10 (2009).
Oh, J. K. & Weiderpass, E. Infection and cancer: global distribution and burden of diseases. Ann Glob Health 80, 384–92 (2014).
IARC. Biological agents. Volume 100 B. A review of human carcinogens. IARC Monogr Eval Carcinog Risks Hum 100, 1–441 (2012).
Bouwes Bavinck, J. N. et al. Human papillomavirus and posttransplantation cutaneous squamous cell carcinoma: A multicenter, prospective cohort study. Am J Transplant 18, 1220–1230 (2018).
Birkeland, S. et al. Cancer risk after renal transplantation in the Nordic countries, 1964–1986. Int J Cancer 60, 183–9 (1995).
Wimmer, C. D. et al. The janus face of immunosuppression - de novo malignancy after renal transplantation: the experience of the Transplantation Center Munich. Kidney Int 71, 1271–8 (2007).
Rama, I. & Grinyo, J. M. Malignancy after renal transplantation: the role of immunosuppression. Nat Rev Nephrol 6, 511–9 (2010).
Hortlund, M. et al. Cancer risks after solid organ transplantation and after long-term dialysis. Int J Cancer 140, 1091–1101 (2017).
Hussain, S. K., Sundquist, J. & Hemminki, K. The effect of having an affected parent or sibling on invasive and in situ skin cancer risk in Sweden. J Invest Dermatol 129, 2142–7 (2009).
Syrjanen, S. Current concepts on human papillomavirus infections in children. Apmis 118, 494–509 (2010).
Koskimaa, H. M. et al. Human papillomavirus genotypes present in the oral mucosa of newborns and their concordance with maternal cervical human papillomavirus genotypes. J Pediatr 160, 837–43 (2012).
Li, X. & Hemminki, K. Cancer risks in women who had children with different partners from the Swedish Family-Cancer Database. Eur J Cancer Prev 11, 433–8 (2002).
Hemminki, K., Ji, J., Brandt, A., Mousavi, S. M. & Sundquist, J. The Swedish Family-Cancer Database 2009: Prospects for histology-specific and immigrant studies. Int J Cancer 126, 2259–67 (2010).
Ji, J., Sundquist, K., Sundquist, J. & Hemminki, K. Comparability of cancer identification among Death Registry, Cancer Registry and Hospital Discharge Registry. Int J Cancer 131, 2085–93 (2012).
Hemminki, K. et al. Surveillance bias in cancer risk after unrelated medical conditions: example urolithiasis. Sci Rep 7, 8073 (2017).
Acknowledgements
Supported by Deutsche Krebshilfe, the Swedish Research Council (2014-2517, 2014-10134 and 2016-01176) and ALF funding from Region Skåne.
Author information
Authors and Affiliations
Contributions
K.H. had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. Study concept and design: K.H., O.H. and A.F. Statistical analysis: L.Z. and G.Z. Acquisition, analysis, or interpretation of data: K.S., J.S., K.H., O.H. and A.F. Drafting of the manuscript: K.H. Critical revision of the manuscript for important intellectual content: A.F., O.H. and G.Z. Final approval of the manuscript for publication: all authors.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Zhang, L., Hemminki, O., Zheng, G. et al. Comparison of Familial Clustering of Anogenital and Skin Cancers Between In Situ and Invasive Types. Sci Rep 9, 16151 (2019). https://doi.org/10.1038/s41598-019-51651-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-019-51651-6
This article is cited by
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.