Coronavirus has been with us for months now. What has changed and where are we going?
Months into the pandemic, one in 100 Americans has tested positive for COVID-19.
When the Northeast was in the throes of the coronavirus pandemic in April, there was talk of passing the peak, pushing to reopen the economy, especially in areas that had largely been spared, and getting the country back on track after arguably the biggest public health crisis in a century.
That process started in earnest in May and early results looked encouraging -- death and case rates at first plateaued and then started to decline in New York and states began to reopen, some very rapidly and even though they did not meet White House gating criteria under pressure from President Donald Trump.
That promise has largely evaporated with a record surge of cases being seen in the South and West, the death toll starting to rise once again and hospitals filled to capacity.
The United States has reached another grim milestone, with 3.5 million confirmed COVID-19 cases, according to Johns Hopkins University, one in 100 Americans testing positive for the virus and 40 states, as well as Washington D.C. and Puerto Rico, reporting an increase in case numbers. The COVID Tracking Project reported on July 16, a record number of 71,229 new cases in the U.S.
Almost five months since the World Health Organization officially declared the COVID-19 crisis a global pandemic, many experts are concerned that the flares in cases in parts of the country reflect major setbacks and failings on the federal and local governments' responses, which have been roundly criticized.
Problems such as equipment shortages and shortfalls on testing, which seemed to be in the rearview mirror after April, have reemerged in new hotspots. And debates rage about the highly political issue of mask-wearing, despite most scientists agreeing that it reduces transmission and even the risk of severe infection for individuals. This is not to mention the lack of clarity about the upcoming school year and how this will affect both children, their parents and the economy at large.
On the other hand, we have learned a lot about the coronavirus, are progressing towards therapeutics and vaccines to help combat the novel disease. The medical community appears to be getting better at treating those who are sick and many in the U.S. have adopted infection-control measures like social distancing, mask-wearing, hand washing and working from home when possible.
But experts interviewed by ABC News warn that for the time being, we remain at the brink, with a long and dangerous road ahead.

'Back in disaster mode'
"There are hotter spots, but everywhere is on the upswing," said Dr. Mathew Heinz, a hospitalist and internist who practices in Tucson, Arizona, one of the nation's newest hotspots.
The most concerning regions "are those where the percent positivity of testing is rising -- and these are places which usually overlap with areas where you see hospitals using more of their capacity for coronavirus patients," added Dr. Amesh Adalja, a senior scholar at Johns Hopkins Center for Health Security, specializing in emerging infectious disease, pandemic preparedness and biosecurity.
Florida recently hit a record of 15,000 cases in one day, "which obliterates records in most countries," said Heinz. He said that at his hospital in Pima County, Arizona, they are almost out of morgue space and thinking about new alternatives to refrigerate and preserve deceased bodies.
"We are back in disaster mode," he added. "All of our facilities had to expand the places within the hospital where we can see COVID-19 patients and you can see that across the state."
In Arizona, the seven-day average test positivity rate hit almost 25%, which, according to Heinz, indicates an "unmitigated spread of the virus" and shows that not enough mild to low-risk cases are being tested.
Many of these new hotspots are in states that were not hit very hard by the virus early in the U.S. epidemic.
"They were spared earlier on and they thought it wasn't something that could happen in their state, and that influenced their behavior," said Adalja. As they watched other states, like New York, weather the COVID-19 storm, these local government officials were "resistant to the concept of requiring any public health regulatory measures like statewide mask orders or lockdowns or fully closing bars restaurants and beaches," Heinz said.
In his state of Arizona, he said, "We did a loosely-enforced lockdown for several weeks, briefly extended and then rushed the opening. There was no phased reopening."
Controlling the virus relies on a heavy investment in testing, tracking and isolating cases, Adalja said.
Testing resources and capacity are major issues nationally, especially in the country's newest hot spots. For example, major diagnostic companies like Quest are reporting delays in result turnarounds. "We are definitely not doing enough tests on a daily basis," said Heinz on the state of Arizona. According to the COVID-19 Tracking Project, Arizona did approximately 14,000 tests on July 15, but Heinz said they should be doing about 75,000.
"It continues to frustrate the entire response," he added, "If you think about it as a war, how are we supposed to figure out where the enemy is to target our resources."
Dr. Anthony Fauci, the country's top infectious disease doctor, said in a recent interview with The Hill that states seeing a resurgence of cases should consider pausing their reopening process. He said states can do "very fundamental things," like closing bars, wearing masks and maintaining social distancing to help curb the spread of the virus. "We went from shutting down to opening up in a way that essentially skipped over all the guideposts. That's not the way to go. We've got to rethink that and do it differently," he said.
Most recently in California, Gov. Gavin Newsom announced major changes, ceasing indoor operations in settings like restaurants, wineries and movie theaters. Counties on the state's "watch list" must also close places like fitness centers, worship services and malls.
On the other hand, New York, the epicenter of the virus early on and the state with a death toll that far surpasses the others, appears to have managed to get a handle on the infection with just several hundred new cases diagnosed a day compared to thousands at the peak and just a handful of deaths.
New York was under a stay-at-home order from late March through early June and is going through a slow, phased reopening, with each region having to meet infection gating criteria. Masks are required in public as is social distancing. Earlier in July, Connecticut reported zero coronavirus deaths for the first time since March.

Scientists learn more about the virus and how to fight it
Even amidst a surge of cases from late June to early July, deaths due to COVID-19 trended downwards across the nation. But experts say the optimism that engendered was premature as the national death count most recently started trending upwards again.
Dr. Angela Rasmussen, a virologist at Columbia University, said there is no conclusive evidence that the virus has mutated in any dramatic way or has changed to become less or more severe. "Looking at the national data can be misleading, but if you look at the hotspots, we started to see those curves turn back into an upwards trajectory," she added.
"People think that maybe the virus has changed, but it's important to remember there is a lag" when it comes to reported COVID-19 deaths, said John Brownstein, Ph.D., an ABC News contributor, chief innovation officer for the Boston Children's Hospital and professor of epidemiology at Harvard Medical School.
"We might see a longer lag in this new era where younger people are representing the bulk of the pandemic," Adalja said.
Dr. Fauci, in a recent interview with The Atlantic, said the age range of people that are getting infected today is about 15 years younger than the age range of people who were getting infected a few months ago.
There was some optimism surrounding this because younger people, especially those without preexisting conditions, tended to fare better, but also fear that carelessness or irresponsible behavior would lead to rapid transmission and more vulnerable populations being affected.
Some officials, including the president, also attributed the rise in cases to an expansion in testing, but an increase in hospitalizations and growing case positivity rate belied that argument.
Brownstein added that there is already a worrying change in the mortality trajectory. "We are already starting to see increases," he said. "If you're looking at the national data, we are seeing numbers of deaths that we haven't seen since the beginning of June."
According to the COVID Tracking Project, on July 16, states reported a total of 977 deaths, which is the highest it's been since May 29. Patients hospitalized with COVID-19 also rose to levels that haven't been seen since April 23. Additionally, the organization said, "After experiencing relatively fewer deaths in the spring, the South has entered a new phase."
Experts are, however, hopeful about the medical progress and the record speed in which experimental therapies and treatments have progressed, including for complications that early only led to many hospitalizations and deaths. "Right now we know a lot more about the pathophysiology of disease, meaning we understand the complications like blood clotting pulmonary embolisms, cytokine storms," Adalja said.
"We don't have cures for this type of illness, but we do have treatments and that's what we are working with now," explained Dr. Bill Jaquis, the president of the American College of Emergency Physicians and an attending physician in Aventura, Florida.
In the early days of the pandemic, there was a massive push for mechanical ventilators as a potential life-saving measure for those with low oxygen levels and severe disease. But data indicated that outcomes from those on ventilators was not encouraging. Doctors also had to get a handle on how to treat cytokine storm, the massive immune response that the novel virus sparked in some.
According to Dr. Robert Glatter, an emergency medicine physician at Lenox Hill Hospital, Northwell Health, doctors have established forms of treatments in the past five months that have markedly improved outcomes. These include "more judicious use of noninvasive ventilation and "proning" in selected patients, along with "targeted therapeutics such as Remdesivir, convalescent plasma, [and] selected IL-6 inhibitors for patients experiencing cytokine storm."
The use of the steroid, dexamethasone, also appears promising for patients with severe respiratory distress, but more data is needed to determine when to give the drug to maximize its effects. Scientists are also working on developing experimental monoclonal antibody treatments, which, according to Adalja, “are synthetic antibodies that were very useful in the treatment of Ebola.”

Rapid progress in the race for a vaccine
Scientists across the country and world are now racing against the clock to develop a vaccine that would prevent people from becoming infected in the first place and limit or stop transmission in the population at large. According to the latest update from the WHO, there are now 23 vaccines that have advanced to clinical trials in people and an additional 140 vaccines being studied in the laboratory.
Most recently, Moderna shared promising results from its phase 1 trial, demonstrating that it was relatively safe for all 45 people it was tested on, and induced the production of antibodies against COVID-19.
According to Dr. Paul Goebfert, the director of the Alabama Vaccine Research Clinic at UAB, Moderna and Pfizer's COVID-19 vaccines "are showing neutralizing antibody induction in humans that are higher than what you get with natural infection." Neutralizing antibodies are thought to protect the body from the virus. Goebfert is hopeful that these vaccines will be effective, but admits we need more data.
According to Goebfert, "If we're doing really well, we will have a vaccine that is 60% effective" -- as no vaccine is 100% effective. He is hopeful that when this vaccine comes, "even people that are infected, despite vaccination, will have a less severe disease."
The flu vaccine, by contrast, is generally 40-60 percent effective, according to the CDC, when most of the circulating flu viruses that season are well matched to the flu vaccine and also provides protection against severe cases in those who become infected.
In an interview with The Atlantic, Dr. Fauci said he is hopeful that by the "end of this calendar year and the beginning of 2021, we will have a vaccine that we'll be able to begin to deploy to people who need it. Obviously, the entire population, but with priorities for those who are most vulnerable."
Although Goebfert agreed with Dr. Fauci's estimates, he cautioned that issues such as unexpected side effects or issues with tolerating the vaccine could "derail" the entire process.
Manufacturers in collaboration with the federal government's Operation Warp Speed are also taking unprecedented measures, ramping up production before knowing if the vaccine will, in fact, be effective and safe.
"People underestimate the tremendous challenge to actually manufacture and distribute the vaccine in the quantity that is going to be needed," said Dr. Awi Federgruen, a professor of management and the chair of the Decision, Risk, and Operations (DRO) Division of Columbia University's Graduate School of Business, specializing in supply chain management.
Resource issues that are already emerging -- like a limited supply of glass vials -- may create major bottlenecks that delay production and distribution. "Geopolitical issues and turf battles between countries [of] who gets priority when there is limited supply," he said, will undoubtedly also emerge.
"I think until we have a vaccine we will see periodic flare-ups in different parts of the country that hopefully are better managed and will put hospitals on some degree of stress, but hopefully not to the breaking point," Adalja said.
Experts agree that we now know a lot more about the virus, including how to treat it and different modes of transmission. But many questions continue to emerge, particularly around what level of exposure leads to infection, duration and extent of immunity and potential for reinfection -- all of which have bearing on the possibility of stopping the infection.
"With early studies showing waning immunity after a just a few months following initial infection, the road to achieving immunity will prove to be challenging," Glatter said.
Looking ahead to the future
Experts do not have a crystal ball, but they agree that the virus will be with us for some time and we must adjust to a modified form of normalcy for the foreseeable future. "The virus is going to be with us. It won't be controlled like in Taiwan, that opportunity has been lost multiple times," Adalja said. "It will be constant burn with this virus. [We will] never get it under full control until there is a vaccine. Everyday new people are born that will be susceptible to it."
As a nation, we face a pivotal point in time, where our actions no longer affect just ourselves but our community at large. While many have become more accepting of the risks of COVID-19, a natural outcome of prolonged time and widespread fatigue, maintaining vigilance and adhering to public health measures can change the course of the pandemic on a national level.
Dr. Robert Redfield, the director of the Centers for Disease Control and Prevention, said in a recent interview with JAMA that we all have a role to play in battling the virus: "masking is not a political issue. It's a public health issue. And it really is a personal responsibility for all of us."
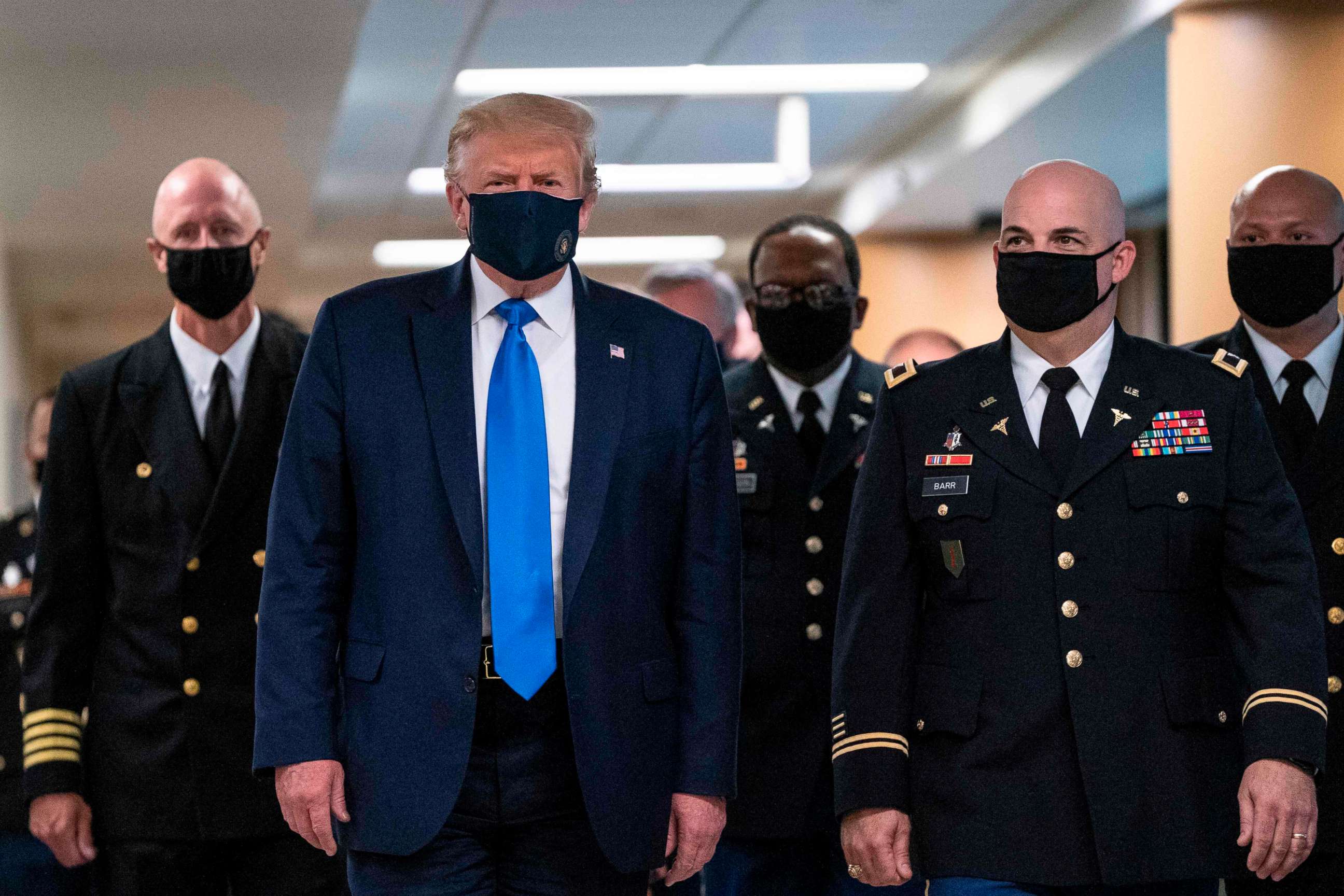
Still, many states and the federal government refuse to mandate masks and roll back state reopening plans to help stem the tide of the virus. Just this month, President Trump, who has been reluctant to wear a mask publicly himself, said that he said he believed COVID would "sort of just disappear."
"The slaughter continues unabated," said Heinz, adding that state governors' reluctance to institute mask-wearing mandates, among other public health regulations, "is more than frustrating its negligence."
"We have to take this seriously, this is a war and we are losing it," he added.
Eden David, who studied neuroscience at Columbia University and is matriculating to Icahn School of Medicine at Mount Sinai later this year, is a member of the ABC News Medical Unit.




