A growing number of women are dying during and after pregnancy in Georgia. The state’s maternal mortality rates have long ranked among the worst in the United States.
The crisis is not new.
And pregnancy, childbirth and postpartum dangers are higher for some in the state than others.
“What is well known is that the disparities by race and ethnicity are persistently high,” said Sarah Blake, an associate professor in the Department of Health Policy and Management at the Emory University Rollins School of Public Health.
Black Georgians are more than twice as likely as white women to experience severe complications or die related to pregnancy, according to the Georgia Department of Public Health.
The top causes of maternal death in Georgia include cardiovascular conditions, hemorrhage and mental health conditions. In 2021, COVID-19 was the second-leading cause.
And, a state board has determined that roughly 85% of maternal deaths are preventable, a number that echoes the national picture.
Georgia’s maternal mortality rate is among the worst in the United States. Families want change. Policymakers and advocates are pushing solutions. We’re exploring the complex factors behind the crisis and what’s being done to address it.
‘It comes back to access’
Why have maternal deaths continued escalating in Georgia, even as the state has dedicated millions of dollars to maternal mortality prevention efforts over the last decade?
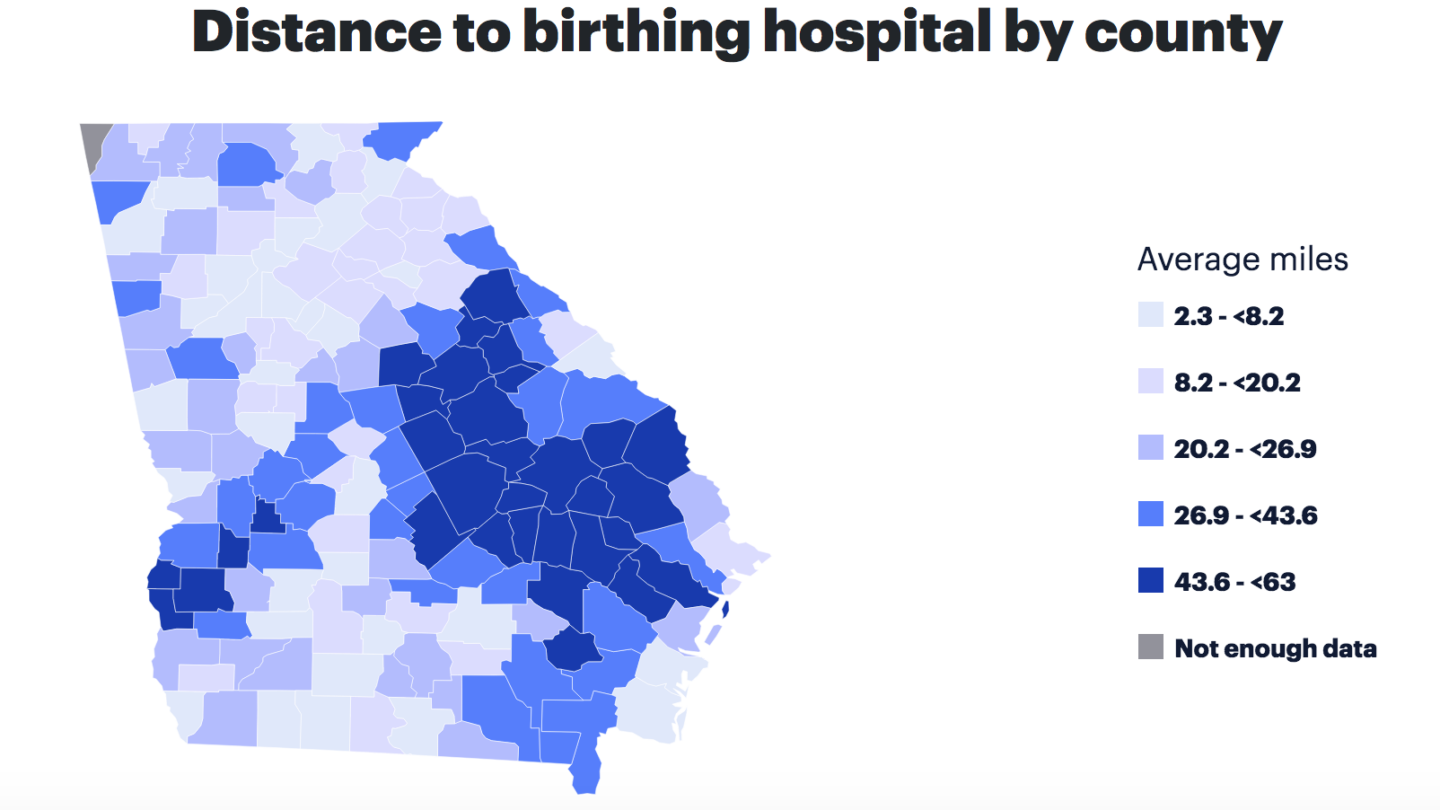
Barriers to accessing timely pregnancy and postpartum health care in the state are major contributors, according to an analysis by the March of Dimes.
More than half of Georgia’s 159 counties have little or no access to maternity care.
“It comes back to access to health care and prenatal care and early care, perinatal care. When it comes to pre-birth post-birth, it comes to better health care for women across Georgia,” said Decatur Democratic state Rep. Mary Margaret Oliver, who serves on the House Public Health Committee. “Poor women, rural women, African-American women do not have the access to medical care that we need with Georgia.”
See Georgia’s 2023 March of Dimes report card.
Oliver is among a coalition of state Democratic lawmakers continuing to push a proposal for full Medicaid expansion in Georgia, which stalled during the last legislative session.
Georgia is one of 10 states that have not fully expanded Medicaid under the Affordable Care Act, which would cover adults with incomes up to 138% of the federal poverty level, or $20,783 for an individual in 2024.
Nonprofit health policy research, polling and news organization KFF has projected more than 430,000 more uninsured Georgia adults would be insured under Medicaid expansion.
Republican Gov. Brian Kemp has opposed full expansion, opting instead for smaller expansion programs, such as Georgia Pathways to Coverage, which offers adults with incomes up to 100% of the federal poverty line Medicaid coverage in exchange for meeting 80 hours per month of work, education or volunteering requirements.
So far, Pathways has seen a sluggish rollout, with fewer than 4,000 people enrolling since it launched last summer.
Kemp has said the program needs more time to grow.
He reiterated his opposition to full Medicaid expansion at a recent live event hosted by the Atlanta Journal-Constitution.
“That’s just not good policy,” Kemp said. “It doesn’t matter if you’re a Republican or a Democrat,” adding that he remains “in the ‘no’ camp” for full Medicaid expansion.
“I think we need to make clear that we need to address both social factors and medical factors. Because it’s not just one or the other.”
Julie Zaharatos, a public health advisor on the CDC Maternal Mortality Prevention Team.
Kemp’s administration has enacted a number of recent initiatives designed to address Georgia’s health care gaps and improve maternal health outcomes.
They include extending postpartum Medicaid coverage up to a year after pregnancy — a policy supported by advocacy groups, including the March of Dimes, for helping to promote equity in maternal and infant health outcomes.
The state Department of Public Health has also launched a home visiting program for women during and after pregnancy that’s now operating in nearly two dozen rural counties across the state.
The causes of a pregnancy-related death are often complex.
They can include doctors or other health care workers missing critical maternal warning signs. A patient’s health before pregnancy also plays a big role.
Communication issues and disparities in treatment during maternity care could also be a factor, according to a recent U.S. Centers for Disease Control and Prevention survey
“There isn’t just one thing that contributed to that tragedy. It’s multiple things. And we really need to use that information to act more systemically on solutions. I think we need to make clear that we need to address both social factors and medical factors. Because it’s not just one or the other,” said Julie Zaharatos, a public health advisor on the CDC Maternal Mortality Prevention Team.
How maternal deaths are tracked in Georgia
Determining which deaths in the state can be counted as pregnancy related is the job of Georgia’s Maternal Mortality Review Committee.
It’s a group of experts — including dozens of maternal health physicians, nurses, epidemiologists and other specialists — that investigates every single reported maternal death in Georgia that occurs within a year of pregnancy.
They pore over patient medical records, autopsies, police reports, social service records and any other available documents, and interview a patient’s family members.
The goal of the investigations is to piece together exactly what led to a woman’s death.
“The committee asks, would she have died if she had not been pregnant? And that guides whether the death was related to pregnancy or not,” said Katie Kopp, who directs maternal health programs at the Georgia Department of Public Health and manages the Maternal Mortality Review Committee.
The committee’s findings help inform state and federal policies on maternal mortality prevention.
Its last report analyzed data between 2019-2021. The next report is expected to come out later this year.
Kopp acknowledged the lag, pointing to the committee’s painstaking process.
“The great benefit of the Maternal Mortality Review Committee is that we can go so in-depth, but it does take time. We have a really extensive review process,” she said. “I do not have concerns that we’re missing deaths.”
Georgia’s committee launched more than a decade ago with support from the CDC.
The agency recommends states operate their own Maternal Mortality Review Committees as one key tactic to combat rising maternal mortality rates.
Still, Georgia’s maternal death rate ranks seventh-highest in the nation, according to a KFF analysis of federal 2018‐2021 data.
What happens next
Health advocates and families affected by pregnancy-related death or a loved one’s severe complications want more action from state and local officials, and the health system to improve the quality of maternal health care and save more lives.
Dr. Natalie Hernandez-Green, an associate obstetrics and gynecology professor at Morehouse School of Medicine, said she is hopeful that Georgia’s maternal health disparities would improve as awareness grows and there is more collaboration to find solutions at the community level.
“What gives me hope is that there are so many people that are working on this, and that we can get to the root causes. We have to work on systems and we have to be really creative on a policy level on how we make systems work for people,” said Hernandez-Green.
As director of the Morehouse School of Medicine Center for Maternal Health Equity, Hernandez-Green is spearheading a national project to document the stories of Black women and other women of color — who face the highest risk for maternal mortality and morbidity.
The project is expanding this year to record the accounts of physicians, nurses and other health care workers, as well as family members in the orbit of a maternal death.
Hernandez-Green said she hopes creating an archive of first-person stories can broaden experts’ understanding of the causes of maternal mortality and morbidity.
“This is a type of methodology that’s congruent with cultural practices of communities of color. You know, how we’ve dealt with past traumas has been through storytelling,” she said. “And so it was a unique opportunity to not just gather data, but do it in culturally congruent ways, and really centering and amplifying the voices of our communities.”
–
This story is part of our WABE series Missing Moms: Inside Georgia’s Maternal Health Crisis. Jess Mador is reporting on it as part of a fellowship with the Association of Health Care Journalists supported by The Commonwealth Fund. It is produced in partnership with the Georgia Health Initiative.