Abstract
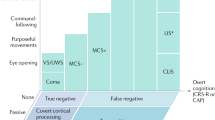
Post-traumatic seizures (PTS) are a common and debilitating complication of traumatic brain injury (TBI) and could have a harmful impact on the progress of patient rehabilitation. To assess the effect of PTS and relative therapy on outcome in the initial phase after TBI, during the rehabilitation process when neuroplasticity is at its highest, we retrospectively examined the clinical data of 341 adult patients undergoing rehabilitation for at least 6 months post-TBI in our neurorehabilitation unit between 2008 and 2019. We correlated through logistic regression the occurrence of seizures and use of anti-seizure medication (ASM) with neurological and functional outcomes, respectively assessed with the Glasgow Coma Scale (GCS) and the Functional Independence Measure (FIM). PTS were documented in 19.4% of patients: early PTS (EPTS) in 7.0%; late PTS (LPTS) in 9.4%; both types in 3.0%. Patients who developed EPTS had an increased risk of developing LPTS (OR = 3.90, CI 95% 1.58–9.63, p = 0.003). Patients with LPTS had a significantly higher risk of worse neurological (p < 0.0001) and rehabilitation (p < 0.05) outcome. Overall, 38.7% of patients underwent therapy with ASM; prophylactic therapy was prescribed in 24.0% of patients, of whom 14.6% subsequently developed seizures. Mortality was associated with a lower FIM and GCS score on admission but not significantly with PTS. The use of ASM was associated with a worse rehabilitation outcome, independently of the onset of epilepsy during treatment. LPTS appear to exert a negative impact on rehabilitation outcome and their occurrence is not reduced by prophylactic therapy, whereas EPTS do not influence outcome. Our findings caution against the generic use of prophylactic therapy to prevent post-traumatic epilepsy in patients with TBI.
Similar content being viewed by others
Introduction
Patients surviving the early stages of traumatic brain injury (TBI) usually have a higher risk of developing disabilities and comorbidities later in life, and TBI has a severe impact on their life span. In this scenario, post-traumatic seizures (PTS) and post-traumatic epilepsy (PTE) are common and debilitating complications of TBI.
In relation to the time-frame of their occurrence, PTS are classified as “early” post-traumatic seizures (EPTS) if they occur within 7 days of the event, and “late” post-traumatic seizures (LPTS) if they occur > 7 days after the event1,2. This cut-off reflects differences in the causal mechanisms and subsequent seizure risk3,4. EPTS, also known as acute symptomatic seizures5, are linked to mechanisms of primary injury that temporarily lower the seizure threshold4. Instead, LPTS are characterized by persistent neurobiological changes attributed to secondary injury with biochemical cascades from epileptogenic mechanisms6,7 conditioning subsequent seizure risk3,4.
Considering the recent clinical redefinition of epilepsy from the International League Against Epilepsy (ILAE)4, the risk of recurrent seizures following a single, unprovoked seizure more than 7 days after TBI is high enough to consider LPTS as an epileptic condition. Therefore, the term LPTS is often used interchangeably with PTE4,8. The overall incidence of PTE in hospitalized patients is about 3–5%9,10, while it represents 10–20% of symptomatic epilepsy in the general population and 5% of all epilepsies6.
Seizures occurring during the acute care phase have a significant impact on the development of additional cerebral damage11. In particular, EPTS appear to increase morbidity and mortality in the early stages following TBI12,13 as well as the risk of developing PTE14,15.
Considering all these factors, early convulsive prophylaxis is commonly used after TBI in clinical practice, although with variable success16. For this reason, it has been a topic of research over the last few decades. While there is evidence of the effectiveness of anti-seizure medications (ASMs) in preventing EPTS, there is no proven benefit of ASM for LPTS and PTE17,18,19. In fact, the recent Brain Trauma Foundation Guidelines20 recommended the use of prophylactic therapy to decrease the incidence of EPTS within 7 days after severe TBI. Historically, phenytoin has been the ASM of choice as prophylactic therapy, but its complications have led to increasing use of levetiracetam as a substitute21. Even on this aspect, there is no clear evidence in the literature22. These inconsistencies could in part be due to the fact that previous epidemiological investigations on PTS were based on heterogeneous populations involving both adults and children3,10,23 and on large-scale multicentre databases where pre-existing epilepsy or previous neurologic injury were not excluded15,24,25.
To address these limitations, we selected only adult patients referred to our neurorehabilitation unit, excluding those with previous neurological conditions such as epilepsy. An advantage of the rehabilitative over the acute setting in assessing patients is the possibility of a more accurate evaluation thanks to the prolonged length of stay of patients. Therefore, in this study, we retrospectively analysed the clinical data of adult patients with TBI from the acute care phase and throughout the subsequent 6 months of inpatient rehabilitation. We focused our analysis within a 6-month period from injury since this period is crucial for the expression of neuroplasticity26. The primary aim of the study was to evaluate the impact of PTS and related antiepileptic drugs on neurological and functional outcomes after inpatient rehabilitation of post-TBI patients. The results of this analysis should give support to clinical decision-making regarding use of prophylactic anticonvulsant therapy in the initial phases after TBI.
Methods
Study design and population
In this observational retrospective study, we included all patients with TBI consecutively admitted to the Neurorehabilitation Unit of ICS Maugeri of Pavia, Italy between January 1, 2009 and December 31, 2018. Collection and analysis of clinical data were performed after approval by the ethics committee of ICS Maugeri (#2214 CE) and in accordance with the ethical standards laid down in the Declaration of Helsinki. Participants, or authorized representatives, signed a written informed consent before admission to neurorehabilitation unit.
The inclusion criteria were the following: (1) age ≥ 18 years; (2) diagnosis of TBI on presentation; (3) admission to a hospital emergency department within 24 h of injury; (4) admission within one month from the injury to the rehabilitation unit to continue clinical care and rehabilitation program; (5) up to 6 months of observation in the rehabilitation setting.
Individuals were excluded from the study if data regarding acute care were not available. We also excluded patients with pre-existing brain injury or other neurological diseases. Furthermore, patients with a history of epilepsy and concurrent use of ASM were not included.
Variables, data sources and measurements
From patients’ hospital electronic records, we collected the following data: age at occurrence of injury, sex, medical history, injury characteristics, fracture site, presence of penetrating TBI, presence of subarachnoid haemorrhage, associated neurosurgical procedures (craniotomy, cranioplasty), neurologic and functional assessments, brain imaging, occurrence of seizures, presence and type of anticonvulsant therapy, death during hospitalization. Seizures were classified according to when they occurred, i.e. during acute care vs. rehabilitation phase. Finally, we collected data from the Glasgow Coma Scale (GCS) and the Functional Independence Measure (FIM) to evaluate, respectively, the neurological and functional outcomes. GCS is used not only to classify the severity of TBI and define its course, but it is also a validated predictor of clinical outcome after TBI27,28,29.
The overall GCS score ranges from 3 to 15; scores 3–8 indicate severe brain injury, 9–12 moderate brain injury, and 13–15 mild brain injury. FIM30 is an 18-item scale designed to measure the patient’s independence in activities of daily living. The severity of disability is evaluated with 13 motor (FIM-M) and 5 cognitive items (FIM-C). In our cohort, the GCS was administrated on arrival at the emergency department (GCS on Arrival; GCSoA). Both GCS and FIM were then administered at admission (T0) and discharge (T1) from the Neurorehabilitation Unit.
We also assessed the TBI characteristics, including type and location of the skull fracture, by radiological imaging. We used the adapted Marshall computed tomographic (CT) classification31 that categorizes injuries into six classes based on: degree of swelling as determined by basal cistern compression and midline shift, and presence and size of focal lesions (i.e. whether the lesion volume exceeds or not 25 cm3).
Anti-seizure medication
Patients in treatment with ASMs were divided into two groups: those who were prescribed ASMs in acute care before the occurrence of seizure (prophylaxis group) vs. those who were prescribed ASMs after the onset of seizures in either the acute or rehabilitation setting (therapy for crisis group).
PTS during acute care and inpatient neurorehabilitation
The presence of seizures during hospitalization was identified via medical records and classified based on time from injury into two classes as previously described7,8: 1–7 days after TBI (early) vs. > 7 days after TBI (late). Physicians examined any paroxysmal clinical event described by patients or eyewitnesses that occurred during hospitalization. Secondly, neurophysiological studies were performed for confirmation.
The documentation of clinical events and the administration of scales during rehabilitation were carried out by the same medical team. Data were collected by the first author and reviewed independently by the second author, with any discrepancies resolved by consensus.
Statistical analysis
Values are expressed as median and interquartile range (IQR) or absolute number and percentage. Data were tested for normality of distribution with the Shapiro–Wilk test and log-transformed when needed in order to correct for skewness. Mann–Whitney and chi-square tests were used for comparisons between groups. Multinomial logistic regression analysis was performed to evaluate associations between presence of epilepsy or use of ASM and anthropometric data, clinical and radiological characteristics of TBI, rehabilitation outcome scores, and mortality. Multiple linear regression analysis was used to evaluate the predictive role of ASM therapy on rehabilitation outcome, adjusted for the presence of seizures. The multilinear models included FIM T1 or ΔFIM as dependent variables and ASM therapy and presence of seizures as independent variables. B coefficients, standard error (SE), β coefficients and significant values obtained from the models were reported.
A value of p < 0.05 was considered as statistically significant. All statistical analyses were performed using SPSS Statistics 21 (IBM Corporation, Somers, NY, USA).
Ethical statement
The study was performed in accordance with the local institutional review board’s approvals.
Consent for publication
All authors have approved the version to be published.
Results
Clinical characteristics of patients with TBI
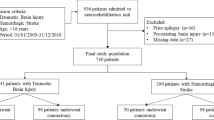
A total of 2082 adult patients were admitted to our neurorehabilitation unit with a diagnosis of acquired brain injury from January 2009 to December 2018 (Fig. 1). Of these, 1549 patients (74.4%) were excluded because of a non-traumatic aetiology, and an additional 192 patients (9.2%) were excluded because they did not meet the other inclusion criteria. The remaining 341 adult patients with mild-to-severe TBI were enrolled in the study. Their demographic characteristics, post-traumatic clinical features and need for primary neurological and/or other surgery are reported in Table 1. Most patients (57.5%) were under 66 years of age at the time of TBI. The majority were males (78.0%), with a male:female ratio of 3.5:1.
Based on the GCSoA, TBI was mild in 11.9% cases, moderate in 22.2% and severe in 65.9%. As regards the localization of the trauma, most patients (61.5%) presented multiple site lesions, with frontal (17.2%) and temporal lobes (13.2%) being the most involved. As a consequence of the traumatic aetiology, approximately half of the patients (51.2%) presented skull fractures, mostly compound skull fractures. In 39.6% of patients, the presence of subarachnoid haemorrhage was detected. Regarding neurosurgical interventions, 38.1% of patients underwent craniotomy and 12.3% cranioplasty. A significant difference between the three classes of TBI severity was found only for age at diagnosis. In fact, patients with moderate and severe TBI were significantly (p < 0.0001) younger compared to those with mild TBI.
Clinical and therapeutic aspects of TBI patients who experienced seizures
During the observation period from acute care to inpatient rehabilitation, 66 patients (19.4%) had reported or documented seizure activity. EPTS were documented in 24 cases (7.0%), LPTS in 32 cases (9.4%) while 10 patients (3.0%) first presented EPTS and then LPTS, two of them being on antiepileptic prophylactic therapy. The clinical and therapeutic characteristics of patients with seizures are reported in Table 1.
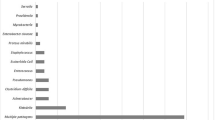
Overall, 132 patients (38.7%) were prescribed ASM. It was prescribed as prophylactic therapy in 82 patients (24.0%), 10 (14.6%) of which subsequently developed seizures (1 EPTS, 9 LPTS and 2 both types). It was prescribed as treatment for crisis in 50 patients (12.2%). Most patients (74.2%) received levetiracetam (II generation ASM). There were no severe drug-related toxic effects during hospitalization and in both groups ASMs were continued for the rest of patients’ stay in the rehabilitation unit. During the 6-month observation period, 42 patients (12.3%) died, but only 6 of them (14.3%) had experienced epilepsy.
Compared to patients without seizures, those who developed seizures were more frequently found to have an evacuated mass lesion according to the adapted Marshall classification (p < 0.01), and a higher prevalence of compound skull fracture (p < 0.05) and they more frequently underwent craniotomy (p < 0.01) and/or cranioplasty (p < 0.05) (Table 2).
We analysed patients with epilepsy according to the type of seizure (EPTS or LPTS or both). Compared to LPTS, patients with EPTS had a significantly higher frequency of diffuse injury grade III according to the adapted Marshall classification and of compound skull fracture (p < 0.05). Moreover, EPTS patients had a significantly higher proportion of compound than depressed skull fractures compared to patients without epilepsy (p < 0.01). On the other hand, patients with LPTS had more frequently undergone craniotomy (p < 0.05) and cranioplasty (p < 0.01), and had a lower CGS (p < 0.05) and FIM (p < 0.05) on discharge.
Finally, comparing patients according to TBI severity, despite the small sample size of patients with mild and moderate TBI, the same differences as above were observed in each group of TBI severity (not shown).
Association between clinical aspects of TBI and risk of seizures
A multinomial logistic regression analysis was conducted to evaluate the association between the clinical aspects of TBI and the risk of seizure onset. All association analyses were weighted for age, gender and severity of TBI. Patients who underwent craniotomy or cranioplasty had a higher risk of seizures than those who did not undergo these interventions (OR = 2.12, CI 95% 1.24–3.66, p = 0.007; and OR = 2.07, CI 95% 1.01–4.25, p = 0.047, respectively), in particular a higher risk of LPTS onset (OR = 2.16, CI 95% 2.13–4.15, p = 0.02; and OR = 3.06, CI 95% 1.40–6.68, p = 0.005, respectively).
We did not find any association between the clinical aspects of TBI and EPTS onset (data not shown). Of note, patients who developed EPTS had an increased risk of developing LPTS (OR = 3.90, CI 95% 1.58–9.63, p = 0.003). Patients treated with ASM had a significantly lower risk of EPTS onset (OR = 0.10, CI 95% 0.01–0.76, p = 0.03). But they did not show a significantly lower risk of developing LPTS (OR = 0.69, CI 95% 0.28–1.65, p = 0.40) or any PTS (OR = 0.50, CI 95% 0.24–1.15, p = 0.12).
Neurological and rehabilitation outcome
At multinomial logistic regression analysis, the presence of seizures was associated with a worse score on GCS (p < 0.05) and FIM (p < 0.01) at the end of inpatient rehabilitation (Table 3).
Patients with LPTS had a significantly higher risk of worse neurological (p < 0.0001) and functional (p < 0.05) outcomes than those with EPTS, in whom this risk did not reach statistical significance.
Further analyses were conducted to compare neurological/rehabilitation outcome parameters between patients according to the use or not of ASMs. As shown in Table 4, patients treated with ASMs had a worse neurological outcome than those not treated.
To further explore the relationship between the use of ASM and outcome, multinomial logistic regression analyses were conducted (Table 5).
Concerning the use of prophylactic therapy, we grouped patients according to onset or absence of seizures during anticonvulsant treatment, with the aim to evaluate whether the association with worse rehabilitation outcome was linked only to the presence of seizures or also to the effect of ASM. Our results showed that the use of ASM, either as a prophylactic or for crisis therapy, regardless of the onset of epilepsy during treatment, was associated with a significantly worse FIM (Table 5). Multiple linear regression analysis (adjusting for the presence of seizures) confirmed that both ASM use and PTS independently predicted rehabilitation outcomes (FIMT1 and ΔFIM) and that the association between FIM and ASM was independent of the presence of PTS (Tables 6 and 7).
We did not find any association between the type of medication used (I or II generation) and neurological or rehabilitative outcome. The same associations between the use of ASM and outcome were found when patients were subdivided according to TBI severity based on the GCSoA (data not shown).
Mortality
Mortality at 6 months from TBI was documented in 42 patients (12.3%) (Table 1). There was no significant difference in prevalence of mortality between the three classes of TBI severity. Lower FIM and GCS scores on admission were associated with higher risk of mortality at 6 months from TBI (OR = 0.94, CI 95% 0.90–0.98, p < 0.01; and OR = 0.39, CI 95% 0.25–0.61, p < 0.0001, respectively). Moreover, mortality was higher in patients > 65 years of age (OR = 8.6, CI 95% 3.71–19.92, p < 0.0001) and in patients who had an evacuated mass lesion on the adapted Marshall Classification (OR = 5.1, CI 95% 1.69–15.56, p < 0.01). We did not find a significant association between mortality and the presence of epilepsy or the use of ASM (data not shown).
Discussion
Incidence and risk factors of PTS
In this study, we evaluated the impact of PTS and relative antiepileptic therapy on neurological and functional outcomes in a large sample of adult patients undergoing rehabilitation after mild to severe TBI and followed for up to 6 months after injury. The incidence of EPTS and LPTS we observed was higher than that found in an earlier study of 199810, but in line with another more recent population-based study15 which had a similar patient profile in terms of TBI severity. The difference in frequency of overall PTS with the earlier study could be explained by the fact that nowadays more patients with moderate-severe TBI survive after severe brain injury. The increasing use of electroencephalography monitoring during acute care also enables clinicians to detect more precisely any type of seizure, thus increasing the diagnostic sensitivity.
Risk factors for PTS have been widely described in the literature15,32,33. In our cohort, the overall risk of PTS was strongly associated with injury characteristics (evacuated mass lesion, compound skull fracture) and neurosurgical procedures (craniotomy and cranioplasty). In particular, patients with a grade III Marshall Classification and compound skull fractures had a higher rate of EPTS, while craniotomy and cranioplasty procedures were significantly associated with LPTS.
Analyzing the associations between clinical aspects of TBI and PTS risk, we found a strong correlation between LPTS and neurosurgery procedures, consistent with the existing literature3,14,15,24,34,35. In line with our findings, a recent study conducted in a paediatric population demonstrated an effect of neurosurgery procedures on seizure risk within the first 6 months after trauma36. Instead, no association was found between the clinical variables and EPTS, although patients who had EPTS had an increased risk of developing LPTS, presumably due to the primary mechanical injury characteristics. We found no age- or sex-related difference regarding the risk of developing PTS at 6 months. Similarly to Rittel et al.15, no correlation between PTS and TBI severity was detected. It is important to underline that our study did not include individuals who were not hospitalized after trauma, possibly limiting the sensitivity of detecting PTS. Finally, in our study, risk of mortality was significantly associated to lower FIM and GCS scores at admission, without any correlation with PTS at 6 months after the event.
Neurological and functional outcomes related to seizures
In terms of recovery after inpatient rehabilitation, only LPTS and use of ASM were significantly related to worse neurological and rehabilitative outcomes, whereas EPTS did not negatively affect the outcome. These findings are consistent with a previous study that demonstrated no difference in neurological recovery at 6 months between patients with or without EPTS23. In our cohort, the occurrence of LPTS was not related to the severity of TBI measured with the GCS on arrival in the emergency department. However, LPTS negatively influenced neurological and functional outcomes at 6 months from trauma, when neuroplasticity is at its highest26. To date a large number of studies have demonstrated that after TBI the primary injury is followed by a cascade of metabolic, biochemical and inflammatory changes36,37,38. These events trigger secondary brain injury resulting in delayed neuronal loss and abnormal neuronal excitability that influence the long-term TBI complications, such as epilepsy36,39,40. This pathological process can also impair the regenerative process after brain injury11, influencing neurological and functional outcome.
Seizures and post-traumatic epilepsy in relation to ASM use
The 2016 guidelines for the management of severe TBI from the Brain Trauma Foundation and the American Association of Neurological Surgeons20 suggest that patients with severe TBI may be treated with ASM soon after trauma to prevent EPTS in that the overall benefits outweigh the risks associated with treatment. These recommendations are heavily based on research by Temkin et al. (1990)14 who demonstrated a significant reduction in the incidence of EPTS with phenytoin compared to placebo14. In this context, an interesting finding of our study is that, although we confirmed that the prophylactic use of any ASM in the 6 months following TBI actually seems to have a protective effect on EPTS, this therapy does not reduce the risk of LPTS. This finding supports the hypothesis that anticonvulsant prophylaxis does not prevent epileptogenic mechanisms coming into play after TBI41,42. Indeed, these mechanisms that may contribute to PTE are still poorly understood, making treatment with ASM of little effect in preventing PTE11,43.
Recent studies have demonstrated no evidence that early treatment with ASMs reduces the risk of LPTS or mortality, whereas it seems to adversely affect functional outcome in the long term14,19,33,41,44,45,46. Levetiracetam, used for early post-TBI seizure prophylaxis, seems to be associated with a shorter length of hospital stay than phenytoin21.
In our cohort, ASMs seem to prevent EPTS but not LPTS, supporting the hypothesis that EPTS and LPTS may have different causal mechanisms39,40. Indeed, EPTS appear to be directly related to the primary mechanical injury, whereas LPTS are a consequence of the secondary process that begins a few minutes after head injury and can persist for months or years39. Moreover, our data showed that the use of antiepileptic drugs appears to be associated with a worsening of functional outcomes, independently of whether therapy is I or II generation and of the occurrence or not of seizures. No toxicity or serious events related to I and II generation ASMs were reported during the observation period. Indeed, in line with recent reviews, our study confirms the same efficacy and safety for both medications with regards to early and late seizure prophylaxis following TBI22.
In summary, our findings raise a further warning against the generic use of prophylaxis with ASM for PTE in the initial phase after TBI. ASM should indeed be limited to those clinical conditions at high risk of LPTS such as patients who have to undergo neurosurgical procedures or, as recommended by the Brain Trauma Foundation guidelines, they should be limited to 7 days after severe head injury.
Study limitations
This study has several limitations mainly due to its retrospective nature. The dataset we used in this study is claim-based and susceptible to miscoding and missing information. In particular, a major limitation is the fact that different protocols were used for the administration of prophylactic therapy in acute care. In this setting, the ASMs were prescribed at physicians’ discretion, probably in relation to the severity of the case. Indeed, our study could not differentiate the use of ASMs in relation to TBI severity or to a clinical indication. This is an inherent confounding factor that requires prospective studies to better understand the effects of ASMs on rehabilitation outcomes.
Another limitation is the high rate of patients with severe TBI in the cohort. However, comparison analysis was conducted in each group of TBI severity and, despite the low sample size of patients with mild or moderate trauma, the same differences as above were observed in each group. Finally, the observation period was relatively short compared to other studies, but our goal was to verify the implications of seizures and epilepsy during the inpatient rehabilitation process and not beyond.
Conclusions
The occurrence of LPTS during rehabilitation negatively influences patient outcomes, and the use of ASM does not seem effective in preventing them. In contrast, prophylactic ASM is more effective in preventing EPTS and appears to have no impact on neurological and functional outcomes and on the risk of late seizures. This study underlines the need to re-examine the use of prophylactic ASM for the prevention of PTE. Based on this retrospective study, prescription of prophylactic ASM after TBI should be limited to those conditions that show evidence of high risk of LPTS or otherwise used for a few days after severe head injury.
References
Lowenstein, D. H. Epilepsy after head injury: An overview. Epilepsia 50, 4–9 (2009).
Antiepileptic Drug Treatment of Posttraumatic Seizures. Brain injury special interest group of the American Academy of Physical Medicine and Rehabilitation Practice parameter. Arch. Phys. Med. Rehabil. 79, 594–597 (1998).
Asikainen, I., Kaste, M. & Sarna, S. Early and late posttraumatic seizures in traumatic brain injury rehabilitation patients: Brain injury factors causing late seizures and influence of seizures on long-term outcome. Epilepsia 40, 584–589 (1999).
Fisher, R. S. et al. ILAE official report: A practical clinical definition of epilepsy. Epilepsia 55, 475–482 (2014).
Beghi, E. et al. Recommendation for a definition of acute symptomatic seizure. Epilepsia 51, 671–675 (2010).
Agrawal, A. et al. Post-traumatic epilepsy: An overview. Clin. Neurol. Neurosurg. 108, 433–439 (2006).
Hunt, R. F., Boychuk, J. A. & Smith, B. N. Neural circuit mechanisms of post-traumatic epilepsy. Front. Cell Neurosci. 18, 89 (2013).
Haltiner, A. M., Temkin, N. R. & Dikmen, S. S. Risk of seizure recurrence after the first late posttraumatic seizure. Arch. Phys. Med. Rehabil. 78, 835–840 (1997).
Chen, J. W. et al. Posttraumatic epilepsy and treatment. J. Rehabil. Res. Dev. 46, 685–696 (2009).
Annegers, J. F. et al. A population-based study of seizures after traumatic brain injuries. N. Engl. J. Med. 338, 20–24 (1998).
Lucke-Wold, B. P. et al. Traumatic brain injury and epilepsy: Underlying mechanisms leading to seizure. Seizure 33, 13–23 (2015).
Englander, J. et al. Mortality in late post-traumatic seizures. J. Neurotrauma 26, 1471–1477 (2009).
Rao, V. R. & Parko, K. L. Clinical approach to posttraumatic epilepsy. Semin. Neurol. 35, 57–63 (2015).
Temkin, N. R. et al. A randomized, double-blind study of phenytoin for the prevention of post-traumatic seizures. N. Engl. J. Med. 323, 497–502 (1990).
Ritter, A. C. et al. Incidence and risk factors of posttraumatic seizures following traumatic brain injury: A traumatic brain injury model systems study. Epilepsia 57, 1968–1977 (2015).
Wat, R. et al. The effectiveness of antiepileptic medications as prophylaxis of early seizure in patients with traumatic brain injury compared with placebo or no treatment: A systematic review and meta-analysis. World Neurosurg. 122, 433–440 (2019).
Young, K. D. et al. A randomized, double-blinded, placebo-controlled trial of phenytoin for the prevention of early posttraumatic seizures in children with moderate to severe blunt head injury. Ann. Emerg. Med. 43, 435–446 (2004).
Christensen, J. et al. Long-term risk of epilepsy after traumatic brain injury in children and young adults: A population-based cohort study. Lancet 373, 1105–1110 (2009).
Thompson, K. et al. Pharmacological treatments for preventing epilepsy following traumatic head injury. Cochrane Database Syst. Rev. 10, CD009900 (2015).
Carney, N. et al. Guidelines for the management of severe traumatic brain injury. Fourth edition. Neurosurgery 80, 6–15 (2017).
Harris, L. et al. Impact of anti-epileptic drug choice on discharge in acute traumatic brain injury patients. J. Neurol. 267, 1774–1779 (2020).
Yang, Y., Zheng, F., Xu, X. & Wang, X. Levetiracetam versus phenytoin for seizure prophylaxis following traumatic brain injury: A systematic review and meta-analysis. CNS Drugs 30, 677–688 (2016).
Lee, T. et al. Early seizures after severe closed head injury. Can. J. Neurol. Sci. 24, 40–43 (1997).
Ferguson, P. L. et al. A population-based study of risk of epilepsy after hospitalization for traumatic brain injury. Epilepsia 51, 891–898 (2010).
DeGrauw, X. et al. Epidemiology of traumatic brain injury-associated epilepsy and early use of anti-epilepsy drugs: An analysis of insurance claims data, 2004–2014. Epilepsy Res. 146, 41–49 (2018).
Wieloch, T. & Nikolich, K. Mechanisms of neural plasticity following brain injury. Curr. Opin. Neurobiol. 16, 258–264 (2006).
Teasdale, G. & Jennett, B. Assessment of coma and severity of brain damage. Anesthesiology 49, 225–226 (1978).
Kouloulas, E. J. et al. (2013) Prognostic value of time-related Glasgow coma scale components in severe traumatic brain injury: A prospective evaluation with respect to 1-year survival and functional outcome. Int. J. Rehabil. Res. 36, 260–267 (2013).
Marmarou, A. et al. Prognostic value of the Glasgow Coma Scale and pupil reactivity in traumatic brain injury assessed pre-hospital and on enrollment: An IMPACT analysis. J. Neurotrauma 24, 270–280 (2007).
Mackintosh, S. Functional independence measure. Aust. J. Physiother. 55, 65 (2009).
Marshall, L. F. et al. A new classification of head injury based on computerized tomography. J. Neurosurg. 75, S14–S20 (1991).
Keret, A. et al. The clinical characteristics of posttraumatic epilepsy following moderate-to-severe traumatic brain injury in children. Seizure 58, 29–34 (2018).
Wang, B. H. et al. Post-traumatic seizures—A prospective, multicenter, large case study after head injury in China. Epilepsy Res. 107, 272–278 (2013).
Englander, J. et al. Analyzing risk factors for late posttraumatic seizures: A prospective, multicenter investigation. Arch. Phys. Med. Rehabil. 84, 365–373 (2003).
Angeleri, F. et al. Posttraumatic epilepsy risk factors: One-year prospective study after head injury. Epilepsia 40, 1222–1230 (1999).
Jassam, Y. N. et al. Neuroimmunology of traumatic brain injury: Time for a paradigm shift. Neuron 95, 1246–1265 (2017).
Pearn, M. L. et al. Pathophysiology associated with traumatic brain injury: Current treatments and potential novel therapeutics. Cell Mol. Neurobiol. 37, 571–585 (2017).
Devanney, N. A. et al. Microglia and macrophage metabolism in CNS injury and disease: The role of immunometabolism in neurodegeneration and neurotrauma. Exp. Neurol. 329, 113310 (2020).
Shlosberg, D. et al. Blood–brain barrier breakdown as a therapeutic target in traumatic brain injury. Nat. Rev. Neurol. 6, 393–403 (2010).
Dadas, A. & Janigro, D. Breakdown of blood brain barrier as a mechanism of post-traumatic epilepsy. Neurobiol. Dis. 123, 20–26 (2019).
Strazzer, S. et al. Late post-traumatic epilepsy in children and young adults: Impropriety of long-term antiepileptic prophylaxis and risks in tapering. Paediatr. Drugs 18, 235–242 (2016).
Dichter, M. A. Posttraumatic epilepsy: The challenge of translating discoveries in the laboratory to pathways to a cure. Epilepsia 50, 41–45 (2009).
Gupta, P. K. et al. Subtypes of post-traumatic epilepsy: Clinical, electrophysiological, and imaging features. J. Neurotrauma 31, 1439–1443 (2014).
Bhullar, I. S. et al. More harm than good: Antiseizure prophylaxis after traumatic brain injury does not decrease seizure rates but may inhibit functional recovery. J. Trauma Acute Care Surg. 76, 54–60 (2014).
Dikmen, S. S. et al. Neuropsychological effects of valproate in traumatic brain injury: A randomized trial. Neurology 50, 895–902 (2000).
Wilson, C. D. et al. Early and late posttraumatic epilepsy in the setting of traumatic brain injury: A meta-analysis and review of antiepileptic management. World Neurosurg. 110, e901–e906 (2018).
Acknowledgements
The authors thank Dr Davide Bertola for the initial phase of data collection of this paper.
Funding
This work was partially supported by the “Ricerca Corrente” Funding scheme of the Ministry of Health, Italy.
Author information
Authors and Affiliations
Contributions
V.P. contributed to the conception and design of the study; acquisition and interpretation of data; drafting of the manuscript. C.M. performed analysis and interpretation of data and contributed to writing the results and the discussion section of the manuscript. All authors contributed to manuscript revision, and read and approved the submitted version.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Pingue, V., Mele, C. & Nardone, A. Post-traumatic seizures and antiepileptic therapy as predictors of the functional outcome in patients with traumatic brain injury. Sci Rep 11, 4708 (2021). https://doi.org/10.1038/s41598-021-84203-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-84203-y
This article is cited by
-
Incidence and predictors of early posttraumatic seizures among patients with moderate or severe traumatic brain injury in Northwest Ethiopia: an institution-based prospective study
BMC Neurology (2024)
-
Insights into epileptogenesis from post-traumatic epilepsy
Nature Reviews Neurology (2024)
-
Post-traumatic epilepsy in Cameroon: a retrospective study in a referral hospital
The Egyptian Journal of Neurology, Psychiatry and Neurosurgery (2023)
-
Functional outcome in patients with traumatic or hemorrhagic brain injuries undergoing decompressive craniectomy versus craniotomy and 6-month rehabilitation
Scientific Reports (2023)
-
Research Progress on the Immune-Inflammatory Mechanisms of Posttraumatic Epilepsy
Cellular and Molecular Neurobiology (2023)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.